What is Aspirin? Aspirin is one of the most popular nonprescription drugs in the world. It is often called a miracle drug, and why not? It’s one of the most common arthritis remedies in existence. It’s reportedly good for everything from pain and inflammation relief to fever reduction, from preventing cardiovascular disease and strokes to helping protect against pregnancy complications, dementia, and even some forms of cancer.
But its benefits don’t stop there. As it turns out, aspirin is also good for recharging your car battery, removing perspiration stains, restoring hair color, and helping cut flowers last longer.1 And it even has its own foundation. No joke! There really is an Aspirin Foundation — aspirin-foundation.com — supported by Bayer® Aspirin, no less.
Aspirin and Cancer
But the reason for today’s newsletter is the recent news concerning aspirin and cancer. For some time, there has been statistical evidence that aspirin may help prevent cancer. Although the evidence is mixed, there have been some studies that indicate aspirin can provide a significant protective effect against breast cancer. For example, a retrospective study of over 80,000 women found upwards of a 28% reduction in breast cancer among women who had used two or more tablets per week for ten years.2 Other studies have been less positive. But there’s even stronger evidence that aspirin may help prevent colorectal cancer, where studies have shown that regular consumption of aspirin may reduce the risk of colorectal cancer by about 40 percent after at least 5 years’ use.3 (This is an especially “interesting” result considering aspirin’s proclivity to intestinal bleeding.)
And now the latest research indicates that the use of as little as one aspirin tablet a month may provide a significant decrease in pancreatic cancer risk, at least according to the results of a case-control study presented just a couple of weeks ago at the American Association of Cancer Research 102nd Annual Meeting.
Xiang-Lin Tan, Ph.D., M.D., discussing the study
In summary, the results of the study showed that people who took as little as just one aspirin a month had a 26 percent decreased risk of pancreatic cancer compared to those who did not take aspirin. The effect was also found for those who took low-dose aspirin for heart disease prevention. Those people had an even better 35 percent lower risk, according to Dr. Tan. It is important to note that the researchers did not see a benefit from non-aspirin NSAIDs or acetaminophen. He also noted that the findings from the study were preliminary, and he did not mean to suggest everyone should start taking aspirin to reduce their risk of pancreatic cancer.
Aspirin
When most people think of aspirin now, they no longer think of pain relief first; they think heart health. But the truth is that aspirin’s heart associated benefits, although blindly accepted as fact, are not necessarily as “clean” as you have been led to believe. Studies have shown that, yes, long-term daily use of low-dose aspirin may indeed lower the risk of “second” heart attacks or strokes caused by blockages, but surprisingly, aspirin does not appear to reduce the risk of dying from these problems. The bottom line is that although aspirin may reduce non-fatal heart attacks, it does not change your odds of dying from a heart attack — and that really is the benefit you’re trying to achieve, isn’t it?
Specifically, the benefits of taking daily aspirin appear to be limited to “men” with previous heart problems who have low or normal blood pressure, not high blood pressure. Women do not seem to benefit. And men with high blood pressure do not seem to realize the benefits. And as a side-effect, they have a higher incidence of internal bleeding problems.
It should also be noted that the aspirin studies indicating cardiovascular benefits for aspirin were done using Bufferin®, not plain aspirin. As Dr. James Howenstine explains, “Four early studies using aspirin to prevent heart attacks had shown no benefit (British Medical Journal 1974 vol. 1 p. 436, Lancet Vol. 2 p. 1313, R. Levy JAMA Feb 15, 1980, R. Peto British Medical Journal 1988 vol. 296 pg. 313-6). Then along came a study on U.S. physicians which used Bufferin (aspirin and magnesium). This study showed no reduction in fatal heart attacks and no improvement in survival rate but there was a 40 % decrease in the number of non fatal heart attacks. The magnesium was ignored and there was a prompt extensive institution of aspirin for prevention of heart attacks.”4
How aspirin works
Virtually all of aspirin’s benefits stem from its ability to inhibit your body’s production of prostaglandins. Prostaglandins are like hormones in that they act as chemical messengers, but they do not move to other places in the body. They work within the cells where they are made. Their role is to direct responses in the human body. For example, prostaglandins play a role in directing the body’s pain and inflammation response to injury. They help control how fast blood clots in response to a wound, or how readily plaque is formed when there is damage to an arterial wall. They also play a role in directing uterine contractions, not to mention your body’s immune response, and even aspects of metabolism. Aspirin and NSAIDS (non-steroidal anti-inflammatory drugs) such as ibuprofen and Motrin work by decreasing prostaglandin levels. They do this by inhibiting the production of the cyclooxygenase enzymes — both COX-1 and COX-2. The presence of COX-2 is required for the production of prostaglandins. Thus, if you inhibit COX 2, you inhibit the production of prostaglandins.
Pain and inflammation relief
 The pain impulse begins at the point of an injury — either external, such as a cut, a burn, or a scrape; or internal such as a knuckle swollen with arthritis. Once the impulse starts, it triggers a number of bio-chemicals to be released at the site of the injury. Some of these bio-chemicals are histamine, bradykinin, Substance P, and several different prostaglandins. Each of these has one or more effects on the body, but many of them are inflammatory — that is, they cause the injury site to swell up. Another action of these bio-chemicals is to stimulate the nerve fibers of pain, the C fibers. (The body actually has three types of nerve fibers: A fibers, B fibers, and C fibers. The main fibers which transmit the pain impulse are the C fibers.) Histamine, bradykinin, prostaglandins, and the other bio-chemicals are actually the stimuli that cause the pain impulse to begin and travel along the C fibers.
The pain impulse begins at the point of an injury — either external, such as a cut, a burn, or a scrape; or internal such as a knuckle swollen with arthritis. Once the impulse starts, it triggers a number of bio-chemicals to be released at the site of the injury. Some of these bio-chemicals are histamine, bradykinin, Substance P, and several different prostaglandins. Each of these has one or more effects on the body, but many of them are inflammatory — that is, they cause the injury site to swell up. Another action of these bio-chemicals is to stimulate the nerve fibers of pain, the C fibers. (The body actually has three types of nerve fibers: A fibers, B fibers, and C fibers. The main fibers which transmit the pain impulse are the C fibers.) Histamine, bradykinin, prostaglandins, and the other bio-chemicals are actually the stimuli that cause the pain impulse to begin and travel along the C fibers.
Thus, reducing prostaglandin production, which aspirin and the other NSAIDs do, can result in decreased pain and inflammation, especially if the prostaglandins are the main cause. It should be noted that aspirin and the other NSAIDS do not directly affect the other pain chemicals; nor do they affect the pain nerve, the C fiber. There are, however, ways to stop pain at those points too. (For more information on how your body’s pain response works and how to naturally relieve that pain, click here.)
Heart disease
Aspirin is unique among the NSAIDs in that it is the only NSAID that inhibits the clotting of blood for a prolonged period (4 to 7 days). Most NSAIDs inhibit the clotting of blood for only a few hours. How does aspirin do this?
Aspirin inhibits both COX-1 and COX-2. We’ve already discussed the function of COX-2 and the role it plays in pain and inflammation — in other words, in response to cell damage and tissue injury. COX-1, on the other hand, has nothing to do with pain; instead, it is primarily a “housekeeping” enzyme, helping to regulate everyday functions in the body — one of which is blood clotting. If you inhibit the production of COX-1, which aspirin does, you reduce the production of platelet aggregating factor thromboxane A2, which means you have less chance of forming blood clots in the arteries — thus a reduced chance of having heart attacks and strokes.
But this brings up the question that we have already alluded to.
Studies have shown that long-term daily use of low-dose aspirin may indeed lower the risk of “second” heart attacks and strokes caused by blockages, but it does not appear to reduce the risk of dying from these problems. The question, then, is what might account for this oxymoron? Again, Dr. Howenstine provides a possible explanation.
“This beneficial effect appears to be completely offset by aspirin’s inhibition of prostacyclin which is a very effective inhibitor of platelet aggregating. In addition, aspirin blocks the enzyme delta-6 desaturase (D6D) which converts linoleic acid to gamma linoleic acid (GLA). Gamma linoleic acid normally is then converted into prostaglandin E1 which has anti-inflammatory properties and appears to have an important role in preventing arteriosclerosis… This enzyme delta-6 desaturase (D6D) cannot be made by most diabetics and failure to produce prostaglandin E1 is believed to be the reason diabetics have devastating arteriosclerosis.”5
Note: COX-1 has one other important function. It is responsible for the proper functioning of the stomach and intestinal lining. Specifically, it promotes the production of the natural mucus lining that protects the stomach, the duodenum, and the small intestine. If you inhibit COX-1, you compromise the integrity of the intestinal tract. We’ll talk more about this later.
Fever
Temperature in the body is regulated by the hypothalamus, located in the brain. When given a trigger for a fever, such as an injury or infection, the body releases prostaglandin E2 (PGE2). PGE2 then in turn acts on the hypothalamus, which generates a systemic response back to the rest of the body, causing the body’s temperature to rise. Higher temperature is not always a bad thing. Among other things, it can directly kill some bacteria, increase the body’s immune response, increase the flow of blood to damaged or infected areas, and increase enzyme activity. As most natural healers know, if you artificially suppress fever when you are sick, you may temporarily “feel” better, but you are actually hampering your body’s ability to get rid of the disease. And in fact, some healers use a technique called the “cold sheet treatment6” to actually force body temperature higher during times of illness to accelerate healing — the exact opposite of “Take two aspirin and call me in the morning.”
Cancer
As it turns out, COX-2 not only plays a role in pain and inflammation, it also plays a role in cell proliferation (probably connected with the body’s need to rapidly replace cells destroyed by injury or infection). Not surprisingly, many cancers display an abundance of COX-2. Thus, reducing production of COX-2 is likely to inhibit the growth of certain tumors. Since aspirin most likely exerts its effect on the formation of adenomas and cancers by inhibiting COX-2 or its downstream effectors, then the use of aspirin should preferentially reduce the risk of those tumors whose growth depends on COX-2 function. And the evidence indicates that it does.7
Aspirin’s history
Over 40 million pounds of aspirin are produced each year in the US alone. That works out to some 200 tabs for every man, woman, and child in America. (I know I don’t use any, so that means some people are eating it like candy to keep those numbers up.) By some estimates, approximately 20-30 million people in the US alone, with the encouragement of their physicians and the aspirin industry, now take aspirin daily for prevention of heart attacks and strokes. In fact, this campaign has become so successful that Bayer® now has to run ads reminding people that aspirin is good for more than just heart attacks. In the most recent ad, an airline passenger complains to a stewardess about back pain. When she recommends an aspirin, he tells her she doesn’t understand — he’s having back pain, not a heart attack. She has to remind him (actually all of us) that aspirin isn’t just for heart health; it’s good for pain too. The mind boggles.
Most people know that aspirin is derived from the active component in white willow bark, salicin, which has been used medicinally for the last several thousand years. The ancient Egyptians used it to relieve pain. Even Hippocrates, the father of modern medicine, reportedly used it to relieve pain and reduce fevers. Aspirin itself, however, is not concentrated salicin. It’s an entirely different molecule. In your body, salicin is converted into salicylic acid. This process was actually discovered and replicated in a lab in the early 1800’s. The problem was that unlike salicin, salicylic acid is both unsettling to the intestinal tract and unstable. It wasn’t until 60 years later, in 1897, that a Bayer® chemist synthesized acetylsalicylic acid. It was both stable, and the acetyl group “covered up” some of the more acid parts of the molecule, making it gentler on the stomach — and thus was born Bayer® aspirin. It quickly became the world’s best selling drug. However, it is important to understand that salicin, the natural healing compound found in white willow bark and synthesized acetylsalicylic acid are not the same thing — not remotely. Salicin does a far better job shielding the body from the acid effects of the molecule.
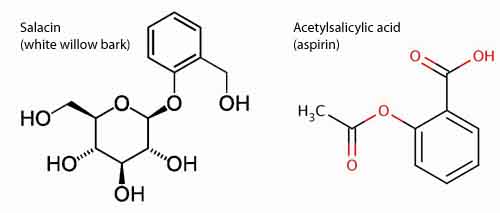
And this difference matters greatly. Salicin provides many of the same analgesic and anti-inflammatory benefits that aspirin does, but it does so without producing gastrointestinal bleeding or any of the other side effects associated with aspirin. This is worth keeping in mind…if you want the benefits without the problems.
Aspirin versus other NSAIDS and acetaminophen
Aspirin is an NSAID. NSAID stands for “nonsteroidal anti-inflammatory,” which simply means that it’s an anti-inflammatory drug that does not contain steroids. This distinction is important. As we’ve already discussed, NSAIDs work by inhibiting the activity of inflammatory bio-chemicals. Like NSAIDs, steroids also reduce the production of inflammatory bio-chemicals, but they also reduce the activity of the immune system by affecting the function of white blood cells. This is not something you want to do when trying to control everyday pain. On the other hand, it’s very useful when trying to control inflammation connected with autoimmune disorders, where the immune system itself is causing the inflammation.
But back to the NSAIDs.
As we’ve already discussed, NSAIDs block the COX enzymes, thereby reducing prostaglandins throughout the body. As a consequence, ongoing inflammation, pain, and fever are reduced. However, since the prostaglandins that protect the stomach and support platelets and blood clotting also are reduced, NSAIDs can cause ulcers in the stomach and promote bleeding. It’s important to understand that NSAIDs vary in their potency, duration of action, and how strongly they inhibit COX-1, and thus their tendency to inhibit the beneficial prostaglandins. The more an NSAID blocks COX-1, the greater is its tendency to cause ulcers and promote bleeding. Some NSAIDs, such as Celebrex® and Vioxx® block COX-2 but have little effect on COX-1 and, therefore, are classified as “selective” COX-2 inhibitors. The theory is/was that selective COX-2 inhibitors cause less bleeding and fewer ulcers than other NSAIDs and are therefore safer than non-selective NSAIDs. But in fact, both Celebrex® and Vioxx® have been associated with significantly increasing the risk of heart attack and stroke. Incidentally, Vioxx® was pulled from the market in 2004 after causing as many as 27,000 deaths. Celebrex® is still sold — and advertised — but with a strong warning on the label.
How did this happen? What was wrong with the theory?
As it turns out, COX-1 and COX-2 enzymes each serve as a “check and balance” for one another. If you selectively reduce one, you unleash the other. This produces a dangerous imbalance which is what has led to the heart attacks, strokes, blood clots, and other cardiovascular side effects linked to selective COX-2 inhibitor use. But worst of all, the evidence suggests that Merck Pharmaceuticals, the maker of both Vioxx and Celebrex, not only knew of the dangers but failed to warn the public and deliberately falsified data used to validate the drugs…and their safety — with full FDA complicity.
Acetominophen, commonly sold under the brand name Tylenol®,is not an NSAID. Although it works through the same bio-chemical pathways as the NSAIDs, it does not reduce inflammation, so it can’t be classified as an anti-inflammatory. It does, however, reduce fever and pain. Acetaminophen is especially dangerous, however, because it damages the liver, which plays a key role in detoxifying the body, regulating cholesterol, and metabolizing drugs.
Aspirin negatives
 Most people think that aspirin is pretty safe except for minor stomach upset, but that’s probably not quite true. It’s not just a question of irritated stomachs. As we’ve already discussed, since COX-1 protects the stomach lining and supports platelets and blood clotting, aspirin can cause ulcers in the stomach and duodenum and promote bleeding once those ulcers have started.8 In fact, even the smallest dose of aspirin causes some degree of intestinal bleeding. But beyond that, too much aspirin actually can poison you, a condition known as salicylism. Symptoms include tinnitus, nausea, vomiting, acute pancreatitis,9 and on some occasions, death. On top of all that, some people are just plain allergic to aspirin — even to the point of anaphylactic shock and death.10
Most people think that aspirin is pretty safe except for minor stomach upset, but that’s probably not quite true. It’s not just a question of irritated stomachs. As we’ve already discussed, since COX-1 protects the stomach lining and supports platelets and blood clotting, aspirin can cause ulcers in the stomach and duodenum and promote bleeding once those ulcers have started.8 In fact, even the smallest dose of aspirin causes some degree of intestinal bleeding. But beyond that, too much aspirin actually can poison you, a condition known as salicylism. Symptoms include tinnitus, nausea, vomiting, acute pancreatitis,9 and on some occasions, death. On top of all that, some people are just plain allergic to aspirin — even to the point of anaphylactic shock and death.10
The bottom line, according to one Spanish study, is that low-dose aspirin alone accounts for between 8.2% and 12.2% of all GI complications and deaths.11 And according to an article in the American Journal of Medicine, “Conservative calculations estimate that approximately 107,000 patients are hospitalized annually for nonsteroidal anti-inflammatory drug (NSAID)-related gastrointestinal (GI) complications and at least 16,500 NSAID-related deaths occur each year among arthritis patients alone.”12 So yes, aspirin can reduce your chances of having a heart attack, but that turns out to be a false benefit since it does nothing to reduce your chances of actually dying from cardiovascular disease — which really is the bottom line you’re after.13 So once again, even though the number of heart attacks is reduced in patients using a daily aspirin regime, the number of strokes and other causes of death increases — not to mention the increased risk of death from other complications. In summary, the side effects from taking aspirin can include:
- Daily aspirin use increases your risk of developing both stomach ulcers and duodenal ulcers. And, if you have a bleeding ulcer, taking aspirin will cause it to bleed more.
- While daily aspirin can help prevent a clot-related stroke, it can increase your risk of a bleeding stroke (hemorrhagic stroke).
- If you’re allergic to aspirin, taking any amount of aspirin can trigger a serious allergic reaction — even to the point of anaphylactic shock and death.
- Overdosing on aspirin can cause tinnitus and even hearing loss in some people.
- If you’re taking regular aspirin and are in an accident or require emergency surgery, you risk excessive bleeding during surgery.
- And finally, alcohol and aspirin don’t mix. In fact, the FDA warns that people who regularly take aspirin should limit the amount of alcohol they drink because of its additional blood-thinning effects and additional potential to upset your stomach.
Aspirin yes, or no?
Before going any further, I probably should mention that the new study demonstrating aspirin’s ability to protect against pancreatic cancer involved a comparison some 1,300 patients — 90 of whom had pancreatic cancer and 1,224 who did not. The press, of course, has been all over this news, like pigs on slop, prompting headlines such as:
- Aspirin Linked to Lower Pancreatic Cancer Risk — WebMD
- Aspirin may lower pancreatic cancer risk — CBS
- Aspirin lowers pancreatic cancer risk — Times of India
How quickly they forget!
Back in 2004, a much larger study conducted by Harvard Medical School of 88,378 female nurses came to just the opposite conclusion: that taking daily aspirin actually increases your risk of getting pancreatic cancer by an astounding 86%!14
At the start of the study, all nurses were cancer free but by 1998, 161 of those women had developed pancreatic cancer. Those who were taking two or more daily aspirin weekly for 20 years, increased their risk of developing pancreatic cancer by 58%, compared to those not taking it. Women who took 14 or more tablets per week had an increased risk of 86%.
Considering that the five year survival rate for pancreatic cancer is only 5% and that the American Cancer Society estimates that more than 30,700 individuals will develop pancreatic cancer this year — and 30,000 of those will die from the disease — perhaps we don’t want to be so quick to jump onboard the new results and start popping aspirin tablets. If nothing else, you’ve got to love the fact that the two studies came to diamettrically opposed conclusions. It’s not like one study found no benefit and the other some — so we could consider the differences merely one of degree. No, one study said aspirin prevents pancreatic cancer, the other said it promotes it — once again confirming one of my favorite themes, that medicine is less scientific than most people think.
But that aside, what should you do if you want the benefits that aspirin supposedly provides, but don’t want the side effects?
Natural alternatives
Aspirin’s chief virtue is that it potentially does so many things — not that it does any one of them especially well. There are alternative health choices that stop platelets from clumping better than aspirin, choices that reduce pain and inflammation better, protect against cancer better, and even reduce fever better — just not all in one miracle pill.
Platelet clumping
Probably nothing works better at optimizing blood quality and reducing the tendency to unhealthy clotting than a good proteolytic enzyme formula, If taken on an empty stomach so it can get into the bloodstream quickly, in less than an hour, a single capsule can totally change your blood profile.
Regular use can easily keep your blood optimized and reduce your chances of having a heart attack. But beyond that, proteolytic enzymes also reduce inflammation throughout your entire arterial system, help dissolve plaque by breaking down the fibrin protein that holds it together, and help repair scar tissue on the arterial walls. All in all, proteolytic enzymes present a far better choice than daily aspirin when it comes to cardiovascular health — particularly when it comes to preventing DVT.
And yes, if you take too much, proteolytic enzymes can reduce the clotting ability of blood to an unhealthy level. You can tell if you’re taking too much if you notice an increased tendency to nose bleeds. But unlike aspirin, at normal doses, proteolytic enzymes do not encourage micro-bleeding of the gastrointestinal tract. If you find you’re taking too much, simply back the dosage down and the problem goes away.
Pain and inflammation
When it comes to pain and inflammation, my first choice would be proteolytic enzymes. Nothing, in my experience, does a better job at reducing systemic inflammation. Best of all, proteolytic enzymes do not work by inhibiting COX enzymes. Instead, they work by accelerating the body’s natural healing processes — instantly promoting better circulation to the area of inflammation, thus reducing edema, and quickly dissolving the bio-chemical residues of injury such as clumps of fibrin, again promoting better circulation and quickly reducing edema and inflammation.
There are also topical oils that will relieve localized deep muscle aches and pains far quicker than aspirin — and for hours longer.
Another choice is to supplement with the omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA), which are a vital link in the body’s anti-inflammatory response. First, they are essential building blocks for prostaglandin E1, the body’s anti-inflammatory prostaglandin. They also stop over-production of COX-2 in the body, as well as slow down production of the pro-inflammatory cytokines. However, there can be a problem if you rely exclusively on vegetable oils such as flax for your source of omega-3.
Omega-3 fatty acids come in three forms: alpha-linolenic acid (ALA), EPA, and DHA. ALA, which is the form found in plants and seeds, is the parent of EPA and DHA, the forms of omega-3 actually used by animals. In fact, in a healthy body, most of the ALA we consume is converted into DHA and EPA. Unfortunately, this process, which is governed by the delta-6 desaturase enzyme, is significantly inhibited (up to 50% or more) by an overabundance of omega-6 fatty acids in the diet. It should be noted that in a healthy diet, the proper ratio of omega-6 to omega-3 fatty acids is 1:1 or 2:1, but in a typical modern diet, all of the refined sunflower oil, corn oil, and soy oil we consume, it runs 20:1, 30:1, and even as high as 50:1. This creates a huge imbalance in favor of omega-6 fatty acids that has to be cleaned up. The delta-6 enzyme is literally “used up” in the desaturation process required to get rid of the excess omega-6 fats that we consume on a daily basis. When the delta-6 enzyme is “used up,” it is no longer available to convert alpha-linolenic acid to its more usable cousins, DHA and EPA. That means, that unless you’re supplementing with fish or krill oil or some other source of EPA and DHA, you’re out of luck. Your body will not be able to manufacture enough prostaglandin E1 to bring inflammation down. And to make matters worse, the delta-6 enzyme is also inhibited by the trans-fatty acids found in all of the partially hydrogenated oils, margarine, and shortening that make up a significant component of the modern diet. But it gets even worse. Delta-6 is further inhibited by high levels of insulin, a problem for the obese and diabetic. In America, two-thirds of the population is now considered overweight and one third is projected to become diabetic. And as a particular insult, diabetics simply cannot produce the delta-6 enzyme at any significant level, which makes their misery even worse, ultimately leading to the arterial inflammation and arteriosclerosis so familiar to most diabetics. And finally, the process of delta- 6-desaturation of linoleic and alpha-linolenic acids slows with aging. Each and every one of these factors can lead to an accumulation of alpha-linolenic acids, which is counterproductive and pro-inflammatory. But there’s more. As it turns out, delta-6 is not only responsible for cleaning out inflammatory fats; it also plays a key role in and of itself in the production of the E1 anti-inflammatory prostaglandin, E1. In other words, even if not the primary cause, low delta-6 desaturase levels are certainly a major contributing factor in the onset of arteriosclerosis.
Which brings us back to aspirin.
Aspirin has a special problem that is never mentioned in its pro heart-health ads. It blocks the delta-6 enzyme, thus preventing production of the anti-inflammatory prostaglandin E1. In other words, aspirin, despite its short term advantages in stopping heart attacks, ultimately contributes to inflammation and thickening of the arteries (arteriosclerosis), which might partially explain why aspirin use ultimately has no effect on improving long term mortality.
Incidentally, an effective method of counteracting the effect of the slowed desaturation of linoleic acid is to provide the 6-desaturated metabolite, gamma-linolenic acid (GLA) directly. The delta-6 desaturation of linoleic and especially alpha-linolenic acid increases dramatically in the elderly with GLA supplementation. The best source of GLA is black currant seed oil. Another good source is evening primrose oil. One other advantage to GLA supplementation is that much of the GLA is converted to DGLA, which competes with arachidonic acid (a byproduct of omega-6 metabolism) and prevents the negative inflammatory effects that arachidonic acid otherwise causes in the body. Everyone eating a typical modern diet should supplement with GLA — especially seniors.
Fever
 Of course, you can always use white willow bark, the original source of salicin to bring down a fever. Also, an extract made from holy basil (AKA tulsi leaves) can be used to bring down fever quite effectively. However, as mentioned earlier, natural healers generally don’t like to force a fever down as they view fever as one of the body’s primary tools for fighting infection and, in fact, often try and increase the fever through the use of hot baths and diaphoretic herbs to speed up the process. As usual, the medical community is slow off the mark on this issue, but research is quietly building in the background in support of this concept.15 Twenty-five years from now, it’s highly likely that doctors will consider using aspirin to reduce fever as counterproductive — but why wait?
Of course, you can always use white willow bark, the original source of salicin to bring down a fever. Also, an extract made from holy basil (AKA tulsi leaves) can be used to bring down fever quite effectively. However, as mentioned earlier, natural healers generally don’t like to force a fever down as they view fever as one of the body’s primary tools for fighting infection and, in fact, often try and increase the fever through the use of hot baths and diaphoretic herbs to speed up the process. As usual, the medical community is slow off the mark on this issue, but research is quietly building in the background in support of this concept.15 Twenty-five years from now, it’s highly likely that doctors will consider using aspirin to reduce fever as counterproductive — but why wait?
Cancer
Trying to prevent cancer by taking aspirin is like plugging a leaky dike with your finger. Its short-term effectiveness is highly questionable (based more on storytelling than hard science), and its long term effectiveness is pretty much doomed since it doesn’t address any of the major contributing factors to the onset of cancer. If you want a better understanding of how to deal with cancer, check out Cancer, the Big Lie.
And if you’re particularly worried about pancreatic cancer, you’re probably better off supplementing with Vitamin D, which has been shown to cut pancreatic risk by nearly half16 with none of the negatives of aspirin…and a whole host of health benefits instead.
Important note: If after reading this article, you decide to stop taking NSAIDs, including aspirin, don’t stop suddenly. Wean yourself off. Stopping daily aspirin therapy abruptly can have a “rebound effect” that can trigger a blood clot that might increase your risk of heart attack or stroke.17 If you’ve been on daily aspirin therapy and want to stop, it’s important to talk to your doctor before making any abrupt changes.
1 Extraordinary Uses for Ordinary Things. 10 Tips That Prove Aspirin’s Amazing. Reader’s Digest Version. 8 April 2011. <http://www.rd.com/home/extraordinary-uses-for-aspirin>
2 Harris RE et al; Women’s Health Initiative. Breast cancer and nonsteroidal anti-inflammatory drugs: prospective results from the Women’s Health Initiative. Cancer Res. 2003;63(18):6096-6101. < http://cancerres.aacrjournals.org/content/63/18/6096>
3 Colorectal cancer prevention. July 2007. Aspirin-Foundation. 8 April 2011. <http://www.aspirin-foundation.com/suitability/documents/Colorectalcancerposition0707.pdf>
4 Howenstine, James, MD. Does Aspirin Prevent Heart Attacks and Strokes? 21 April 2004. NewsWithViews.com. 9 April 2011. < http://www.newswithviews.com/Howenstine/james10.htm>
5 Ibid.
6 Dr. John R. Christopher’s “Cold Sheet Treatment”. Dr. Christopher’s Herbal Legacy. 29 March 2011. <http://www.herballegacy.com/Cold_Sheet.html>
7 Andrew T. Chan, M.D., M.P.H., Shuji Ogino, M.D., Ph.D., and Charles S. Fuchs, M.D., M.P.H. Aspirin and the Risk of Colorectal Cancer in Relation to the Expression of COX-2. N Engl J Med 2007; 356:2131-2142. <http://www.nejm.org/doi/full/10.1056/NEJMoa067208#t=article>
8 A I Lanas, M T Arroyo, F Esteva, R Cornudella, B I Hirschowitz, and R Sáinz. Aspirin related gastrointestinal bleeders have an exaggerated bleeding time response due to aspirin use. Gut. 1996 November; 39(5): 654–660. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1383387>
9 Sidney Sussman. Severe Salicylism and Acute Pancreatitis. Calif Med. 1963 July; 99(1): 29–32. <http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1515161/?page=1>
10 < Aspirin Allergy. FreeMD. 10 April 2011. <http://www.freemd.com/aspirin-allergy/overview.htm>
11 Angel Lanas MD, Maria Angeles Perez-Aisa MD, et al. A Nationwide Study of Mortality Associated with Hospital Admission Due to Severe Gastrointestinal Events and Those Associated with Nonsteroidal Antiinflammatory Drug Use. The American Journal of Gastroenterology (2005) 100, 1685–1693. <http://www.nature.com/ajg/journal/v100/n8/full/ajg2005304a.html>
12 Singh Gurkirpal, MD. “Recent Considerations in Nonsteroidal Anti-Inflammatory Drug Gastropathy.” The American Journal of Medicine, Volume 105, Issue 1, Supplement 2 , Pages 31S-38S. 27 July 1998.) <http://www.amjmed.com/article/S0002-9343(98)00072-2/abstract>
13 Wolff T, Miller T, Ko S. Aspirin for the primary prevention of cardiovascular events: an update of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2009;150(6):405. <http://www.uptodate.com/contents/benefits-and-risks-of-aspirin-in-secondary-and-primary-prevention-of-cardiovascular-disease/abstract/55>
14 Schernhammer ES, Kang JH, Chan AT, Michaud DS, Skinner HG, Giovannucci E, Colditz GA, Fuchs CS. A prospective study of aspirin use and the risk of pancreatic cancer in women. J Natl Cancer Inst. 2004 Jan 7;96(1):22-8. <http://www.ncbi.nlm.nih.gov/pubmed/14709735>
15 MJ Kluger, DH Ringler, and MR Anver. Fever and survival. Science 11 April 1975: Vol. 188 no. 4184 pp. 166-168. <http://www.sciencemag.org/content/188/4184/166.short>
16 Halcyon G. Skinner, Dominique S. Michaud, Edward Giovannucci. et al. Vitamin D Intake and the Risk for Pancreatic Cancer in Two Cohort Studies. Cancer Epidemiol Biomarkers Prev September 2006 15; 1688. <http://cebp.aacrjournals.org/content/15/9/1688.full>
17 Mayo Clinic Staff. Daily aspirin therapy: Understand the benefits and risks. MayoClinic.com. 11 April 2011. http://www.mayoclinic.com/health/daily-aspirin-therapy/HB00073











In your excellent portrayal
In your excellent portrayal of aspirn you mention that it is or can be associated with increased risk of bleeding in the stomach. Isn’t its action as a blood thinner and coagulent inhibiter just as dangerous anywhere were blood flows in the human body? While the tomach may made more susceptable by ulcers, how about other areas of the body such as the eye? Here I’m thinking about macular degeneration, particularly in the aged and semi aged. Fluid mechanics tells us that fluids, particularly thin fluids, have the most potential to leak where the retaining structure is the weakest. Do you agree?
Excellent article, very
Excellent article, very useful information.
Many thanks, Jon.
Great tip on using the
Great tip on using the enzymes to get relief from pain and so many health benefits. I will start doing that very thing. I have them on hand to help digest food, but always forget to take them when I eat. From now on I’ll just take some in the morning, just for the good benefits you spoke of, re getting rid of inflammation, plaque, so much.
Wow. Who would have thunk it!
I'm 60 & had a stent put in
I’m 60 & had a stent put in my heart after a vascular crimp caused 2 heart attacks. Each day I take 5mg-warfrin; 1,800mg-Red Yeast Rice; 40mg-Lowpressor; 1tbs freshground Royal Mace & 2- Omega-3s (highest potency) PER DAY. Oh yes. My blod pressure is 120/69 & I execise with a trainer 4hrs./wk (bike, swimming, free wts.
Will Salacin, DHA, ALA, Magensium or Poleteolytic Enzyme have a harmful interaction with any of the above?
I took th red yeast rice dosabe for 6 mos. & cut my 40mg of Zocor 50%.
Result? All high DLS & Gloucose were under 80 in month 6!
Once again Jon Barron is
Once again Jon Barron is prepared with good information and clarity. I remember my brother saw someone on TV once suggest people take aspirin daily to reduce heart attacks. My brother did, and in 2 days the blood vessels in his eyes were all bloodshot. his eyes were not just a little red, his eyes were completely red. Needless to say he stopped the aspirin and it cleared up.
Nearly 5 years ago I
Nearly 5 years ago I collapsed and when taken to hospital, the same consultant who had treated me years before for a couple of mild heart attacks, and put me on 300mg of aspirin per day and then eventually brought it down to 75mg per day. He told me that I was losing blood because of the Aspirin and I had to receive 4 pints of blood. The aspirin had caused stomach ulcers which then began to bleed. He has me on Clopidogril now, says it’s the same as Plavix which thins the blood but causes no bleeding.. Yet I remember him telling when he first prescribed the aspirin that once I was on these I would never have heart trouble again. How wrong can you be, and yet, most folk, like myself take everything as the Doc says as Gospel. Well, I tell everyone I talk to and if the subject arises, I advise them to get off the aspirin and ask for an alternative. David Glass.
Dear Jon and readers,
I am
Dear Jon and readers,
I am based in the UK and read a flurry of publicity recently concerning the claim that Asprin will help reduce the risk of cancer.
Well I continued to read and dig and further down when most had given up, one journalist asked the scientists and researchers why they thought Asprin may contribute the fighting of cancer, which was not prevalent in society 100 years ago. The answer was both interesting and telling. The answer was that they think the use of modern fertilizers counteracts the beneficial effects of vegetables and that has effected the rate of increase in cancer in our modern society in relation to the increase in modern fertilizer. Asprin helps to chemically replicate the natural effects of vegetables.
Personally I think most vegies should be eaten raw, as we did as hunter-gatherers and in that way full beneficial effects from them.
By the way, try an experiment for yourselves. Get one normal carrot strait from the local store and get one ‘organic’ carrot and leave them on the sideboard for a week or so. The organic carrot dries up and shrivels, the standard fertilizer fed carrot will turn to mush and liquid and leek across your sideboard.Ughhhh
Carry on the good work
Best wishes
John
Excellent read! I have been
Excellent read! I have been using both proteolectic enzymes as well as serrapeptase enzymes for the last year with what I believe to be successful results.
Thanks for an excellent
Thanks for an excellent article. I learned about proteolytic enzymes from an OMD over 10 years ago after my husband had a couple of stents inserted in his anterior descending artery. We did not want to use prescriptive blood thinners but knew about the necessity of preventing clots. So we took the OMD’s advice and started using Wobenzyme, later added Nattokinase, sometimes Serrapeptase,and bromelain, and it has worked beautifully with no problems. He takes it with a teaspoon of Buffered C (1000 mg) and 500 mg of time-release NAC to boost his immune system.
Jon, Life Extension touts the
Jon, Life Extension touts the benefits of a low dose aspirin. Why is this? They are a reputable organization. I don’t take aspirin myself but I have been considering it recently. Now I am not sure.
There re too many natural
There re too many natural blood thinners (Bromelain & Quercetin, etc.) to even consider taking aspirin, with all its side effects. One of the latest is the effect on your eyes. Check it out; don’t take my “word” for it. Also, there are a multitude of foods that thin the blood and address pain. Do your “homework,” and find out that which you don’t know at this point in time concerning this issue.
Many thanks, I learned a lot.
Many thanks, I learned a lot. I am a retired chemist and understood most of what you said. I have always thought the birch bark extract was salicylic acid. Was surprised to see no aromatic ring and 5 asymmetric centers. I was also aware of the problem of the gamma 6 to gamma 3 ratio but did not understand the reason. I have switched to using olive oil from sunflower oil and am investigating sourcing coconut oil for cooking as well. I also take about 10ml (2tsp) of cod liver oil per day. Hopefully that will sort out my gamma 3 to 6 ratio. Alas, it is not always possible to eat properly so I take multitudinous supplements. There is no simple solution for everything.
There exists an Indian Herb
There exists an Indian Herb by the name “Ashwagandha” claimed to be a good alternative to Aspirin…..is that true? It is also a good nutritional supplement, they say !
Thanks for the information. I
Thanks for the information. I enjoy the level of detail which admits that your readership may not be avid scientists but that some facts are understandable. You are a highly valued voice of reason in the alternative health confusion.
Once again, thank you.
Thank you a most informative
Thank you a most informative newsletter and side bar leads etc. Answers many questions I have long harboured.
Thanks for the informative
Thanks for the informative article! Your research, recommendations, and discernment are greatly appreciated.
Just had a heart attack a
Just had a heart attack a month ago, taking 3 stents to open the blocked area. My cardiologist wants me to take Plavix AND a low dose aspirin every day–plus a statin drug, which I don’t tolerate well. How can I convince him that the aspirin is not necessary and that I could get equal results with policosinol and/or red rice yeast instead of the statin? Any suggestions?
why need convince your
why need convince your cardiologist? take what you think is right for you – it`s you who has to bear the consequences, not your doc.
you also might choose another cardiologist.
normally plavix and aspirin should not be taken together.
it is also wise to take plavix no longer than a year, as afterwards the likelyhood of getting lymphatic cancer increases 5fold (my father took it for about 4 to 5 years after which he developed non-hodgkin`s lymphoma).
a statin drug does have some health benefit, but only in small doses (10mg/day) – in such doses it has a good anti-inflammatory affect and its side-effects, stemming from inhibiting the production of coenzyme q10 and an abnormal reduction of cholesterol (weakness of muscles and heart, bad memory, cancer) are minimal. but one should always take co-enzyme q10 as a supplement when taking a statin drug – you should also take q10 while taking red rice yeast.
My father is 62 years old.
My father is 62 years old. Three years ago he had his second heart attack. His doctor told him that unless he had a triple bypass and took plavix that he was a walking dead man. He refused to let them operate on him and instead did research. He has been taking Natokinase, COQ-10, and has recently started taking VEMMA, VEMMA is actually an acronym that stands for Vitamins, Essential Minerals, Mangosteen, and Aloe. It is a drink that you drink 4 ounces each day. He has seen positive results in his blood work, and guess what… He is not on any harmful drugs with all the negative side effects. I just thought you may want to check out an alternative option. If you choose to try this out I would consult with your doctor and take this in conjunction to what your doctor has prescribed.
Well written article with so
Well written article with so much depth. Helped me out a lot with my term paper research. Thanks Ted
Thank you for this great
Thank you for this great article. It’s very informative and interesting. It also answeres me in some questions.
Link
Here are some interesting
Here are some interesting links:
11/09 BBC article re. a recent UK Drugs and Therapeutics Bulletin opinion on aspirin: http://news.bbc.co.uk/go/pr/fr/-/2/hi/health/8338763.stm
http://www.telegraph.co.uk/health/healthnews/6114302/Aspirin-does-more-harm-than-good-in-healthy-people-research.html
http://www.reuters.com/article/2007/05/08/us-risks-idUSN0737156120070508 Is taking aspirin as risky as driving?