Perhaps you saw the headlines.
“Evolocumab significantly reduces risk of cardiovascular events.” Science Daily1 American College of Cardiology. “Evolocumab significantly reduces risk of cardiovascular events.” ScienceDaily. March 17, 2017. (Accessed 22 Mar 2017.) http://www.sciencedaily.com/releases/2017/03/170317132012.htm
“New drug shows promise in preventing heart attacks.” NHS Choices2 Bazian. “New drug shows promise in preventing heart attacks.” NHS Choices. March 20, 2017. (Accessed 22 Mar 2017.) http://www.nhs.uk/news/2017/03March/Pages/New-drug-shows-promise-in-preventing-heart-attacks.aspx
“Evolocumab Added to Statins Cuts CV Events.” Medscape3 Deborah Brauser. “Evolocumab Added to Statins Cuts CV Events in FOURIER Trial.” Medscape. March 17, 2017. (Accessed 22 Mar 2017.) http://www.medscape.com/viewarticle/877348
Very impressive at first glance, but what are those lines from Gilbert & Sullivan’s HMS Pinafore?
Things are seldom what they seem,
Skim milk masquerades as cream;Very true,
So they do.
As it turns out, when we look at the study in question, it seems that we may have been Pinafored.
Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease–The Study
According to the cholesterol theory of heart disease, low-density lipoprotein (LDL) cholesterol is a “well-established and modifiable risk factor” for cardiovascular disease. With that in mind, doctors are forever looking for ways to “modify” it downward, ever downward. In mid-March of 2017, the New England Journal of Medicine published the results of the first rigorous test of evolocumab (sold under the brand name Repatha®).4 Sabatine MS, Giugliano RP, Keech AC, et al. “Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease.” NEJM. March 17, 2017. http://www.nejm.org/doi/full/10.1056/NEJMoa1615664#t=article Evolocumab is a monoclonal antibody that inhibits the PCSK9 enzyme. Whereas statin drugs work by blocking the HMG-CoA reductase enzyme in your liver that actually is responsible for making cholesterol, PCSK9 inhibitors suppress the particular gene that regulates how much cholesterol your liver can remove from the bloodstream.
According to the study, which cost close to $1 billion, when evolocumab is added to statin therapy (note: it is not used by itself but in conjunction with statin therapy), it lowers LDL cholesterol levels an additional 59% from baseline levels as compared with placebo–from a median of 92 mg per deciliter to 30 mg per deciliter. Also, according to the study, evolocumab significantly reduces the chances that high-risk patients will have a heart attack or stroke. (Note: evolocumab, the drug used in the study, is made and sold by Amgen. Alirocumab, a similar drug, is made by Sanofi and Regeneron. They are all of the same family. Evolocumab was used in the study because Amgen paid for the study.)
As enthusiastically quoted in the New York Times:5 GINA KOLATA. “Cholesterol-Slashing Drug Can Protect High-Risk Heart Patients, Study Finds.” New York Times. MARCH 17, 2017. (Accessed 20 March 2017). http://www.nytimes.com/2017/03/17/health/cholesterol-drugs-repatha-amgen-pcsk9-inhibitors.html
“This is like the era of the statins coming in,” said Dr. Eugene Braunwald, a cardiologist at Harvard Medical School who was the founding chairman of the research group that conducted the study, but was not an investigator on it. Like statins, which were introduced in the 1980s, the new class of drugs has the potential to improve the health and longevity of millions of Americans with heart disease, the nation’s leading killer, accounting for one in four deaths.
“It’s a new ballgame,” he said.
And again, according to the New York Times:
For cardiologists, the study was a crucial test of a long-held hypothesis: the lower the level of cholesterol in the blood, the better.
The results support that hypothesis. There seemed to be no floor to the benefits of cholesterol lowering, at least down to the stunningly low levels achieved in the study. The lower the LDL, the lower the risk, with no leveling off of the linear relationship.
Well, I guess that means that we’ll all soon be on evolocumab, yes?!!!
Not necessarily. There are a few Blue Screens of Death6 http://en.wikipedia.org/wiki/Blue_Screen_of_Death in evolocumab’s basic operating system, as it were.
Cost Benefit Doesn’t Work
First off, cost is going to be an issue. Repatha has a list price of $14,523 a month!!! Statin drugs, which are now available as generics cost a tiny fraction of that (maybe $30-60 a month). Insurance companies have so far been “disinclined” to pay for Repatha, or any of its relatives, without evidence it produces benefits that warrant the higher costs. However, with 11 million users projected out of the gate if insurance covers the costs, the potential profits are astronomical. No wonder Amgen was willing to spend a billion dollars to conduct the study to convince both the medical community and the insurance companies to get behind it. So, what results did they get?
Even that Benefits Are Questionable
If you look at the numbers the way Amgen spun them, they look pretty good.
Results showed that the drug cut heart attack risks by 27% over the course of the study, which followed patients for an average of two years. And it cut the risk of stroke by 21%. Put those two stats together, and Repatha patients saw a 19% reduction in risk of all cardiac events for the first year and 33% after that. So far, so good.
But if you do a Joni Mitchell and look at those numbers from the other side, you find they tell a very different story. First, the absolute reduction in the risk of a heart attack or stroke is far, far less. According to Amgen, it’s only 1.3 percent at two years and 2 percent at three years. That doesn’t sound anywhere near as good, and even those numbers are highly spun as they sidestep a key piece of data mentioned in the study.
To quote from the study’s results section.
“In terms of individual outcomes, evolocumab had no observed effect on cardiovascular mortality…There were reductions of 21 to 27% in the risk of myocardial infarction, stroke, and coronary revascularization but no observed effect on the rates of hospitalization for unstable angina, cardiovascular death or hospitalization for worsening heart failure, or death from any cause.”
In other words, evolocumab may lower cholesterol levels and reduce the “number” of cardiovascular events, but it has ZERO impact in terms of how often you go to the hospital and, more importantly, your odds of dying. To put it simply, your chances of dying ere exactly the same whether you use the drug at a cost of $174,000 a year or not. The bottom line is that insurers would have to pay nearly $1 million for every single “event” that the drug was able to prevent in a patient–without saving a single life or preventing a single hospitalization. (Incidentally, this is true of statin drugs too. Statins may reduce your chances of having a heart attack, but they don’t change your odds of dying.)
This was not lost among analysts, pricing experts, and investors. After the study’s data was presented at the American College of Cardiology meeting, Amgen’s shares immediately dropped by more than 6%.
Ouch!
And What About the Negatives Associated with Pushing Cholesterol that Low
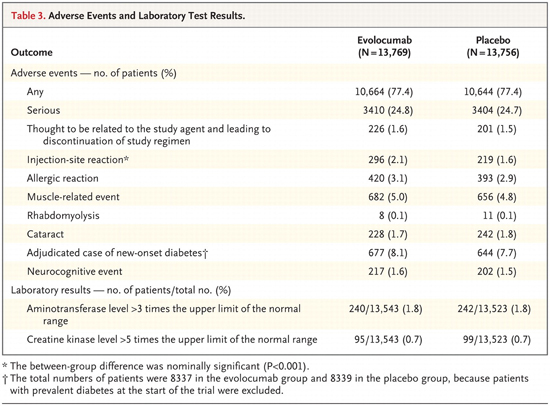
According to the study, there were no significant differences in adverse events between those using evolocumab and placebo. (Remember that the placebo group was using statin drugs, just not the evolocumab, as evolocumab doesn’t replace statins; it merely supplements them.)
But let’s talk for a moment about the adverse effects that aren’t on this list–events that also are specifically related to low cholesterol levels. Keep in mind that despite its reputation, cholesterol (even some forms of LDL cholesterol) isn’t bad for the body at proper levels; in fact, it’s essential. And we’re talking about LDL cholesterol. Before we go any further, though, we need to clear up a misapprehension promoted by the medical community. They have marketed the idea that HDL is good cholesterol and that LDL is bad cholesterol, but that’s like defining an H-bomb as something that goes boom–a valid definition, but ultimately useless because of its lack of detail. The truth is that HDL is labeled good because it transports excess cholesterol from peripheral tissue TO the liver for excretion. And yes, that’s good–especially because modern diets crush liver function, thereby pushing cholesterol levels upward. LDL, however, is only bad in excess and when it’s of a certain type. LDL transports cholesterol FROM the liver to all the tissue and cells outside the liver where it is used for all the essential things that cholesterol does in the body.
For example, cholesterol serves as the raw material for the synthesis of all the major hormones in your body: testosterone, estrogen, progesterone, and cortisol. Testosterone, as we discussed in our last newsletter, is synthesized out of cholesterol in both men and women. If your cholesterol levels are too low, you don’t make enough testosterone–and that has serious health consequences. And in fact, studies show that low free testosterone is a likely predictor for muscle loss.7 Yuki A, Otsuka R, Kozakai R, et al. “Relationship between low free testosterone levels and loss of muscle mass.” Sci Rep. 2013;3:1818. http://www.ncbi.nlm.nih.gov/pubmed/23660939
Then there’s your brain and central nervous system (CNS). Cholesterol is vitally important for brain function. 25% of the cholesterol in your body is found in your brain. And while your brain represents only about 2-3% of your total body weight, your brain and nerves are about 20% cholesterol by weight. Essentially, if your cholesterol is too low, your central nervous system starts having problems with things such as membrane function and antioxidant protection. At this point, you might be asking yourself, “If this is true, wouldn’t this show up in some common health issues related to the CNS?” And it does.
Low levels of LDL cholesterol have been associated with an increased risk for depression,8 Steegmans PH, Hoes AW, Bak AA, et al. “Higher Prevalence of Depressive Symptoms in Middle-Aged Men With Low Serum Cholesterol Levels.” Psychosomatic Medicine: March/April 2000 – Volume 62 – Issue 2 – pp 205-211. http://journals.lww.com/psychosomaticmedicine/Abstract/2000/03000/Higher_Prevalence_of_Depressive_Symptoms_in.9.aspx higher mortality rates, especially in the elderly9 CAROLINE WELLBERY. “Low Cholesterol Levels Associated with Increased Mortality.” Am Fam Physician. 2005 Nov 1;72(9):1859-1860. http://www.aafp.org/afp/2005/1101/p1859.html –and suicide.10 Wu S, Ding Y, Wu F, Xie G, Hou J, Mao P. “Serum lipid levels and suicidality: a meta-analysis of 65 epidemiological studies.” J Psychiatry Neurosci. 2016 Jan;41(1):56-69. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4688029/ Even more interesting is a study just published in the Journal of Affective Disorders that found an association between high levels of HDL (you know, the “good” cholesterol) and increased levels of depression and suicidality.11 Oh J, Kim TS. “Serum lipid levels in depression and suicidality: The Korea National Health and Nutrition Examination Survey (KNHANES) 2014.” J Affect Disord. 2017 Apr 15;213:51-58. http://www.ncbi.nlm.nih.gov/pubmed/28189965 Try telling that to your doctor.
Another Nail in the Cholesterol Theory of Heart Disease
 I have talked about the holes in the cholesterol theory of heart disease many times, so I am not going to repeat them here today. What I am going to do, though, is explain to you why this recent study, contrary to the headlines you may have seen, does not represent a victory for cholesterol lowering drugs but, rather, once again rips open a gaping hole in the theory. Before we go there, however, let’s do a quick review of cholesterol.
I have talked about the holes in the cholesterol theory of heart disease many times, so I am not going to repeat them here today. What I am going to do, though, is explain to you why this recent study, contrary to the headlines you may have seen, does not represent a victory for cholesterol lowering drugs but, rather, once again rips open a gaping hole in the theory. Before we go there, however, let’s do a quick review of cholesterol.
Cholesterol is a fat-soluble steroid. In fact, it is the most abundant steroid in the body. Far from being harmful, when properly regulated, it is a critically important molecule. As a fat-soluble molecule, however, cholesterol cannot easily be carried in the blood–a water based medium. Therefore, the body converts cholesterol into water-soluble molecules known as lipoproteins so it can be transported. Lipoproteins are comprised of a core of fats (lipids) including cholesterol, an outer shell made from a phospholipid which renders the particle soluble in water, and a surface protein molecule (apolipoprotein) that allows tissues to recognize and take up the particle. Lipoproteins are characterized by their density. In simple terms, LDL cholesterol is what your liver produces to travel out “into” your body to be utilized by your organs and cells. And HDL cholesterol is what your body produces in order to capture excess cholesterol in your bloodstream and escort back to your liver and out of your body. Which brings us to our first surprise: you need LDL.
LDL cholesterol is not one thing. It actually comes in two (and possibly four) different flavors.
And now we come to our second surprise: LDL cholesterol is not one thing. It actually comes in two (and possibly four) different flavors: a big, fluffy form known as large LDL, and as many as three increasingly dense forms known as medium, small, and very small LDL (aka VLDL).12 Francisco Lopez-Jimenez. “VLDL cholesterol: Is it harmful?” Mayo Clinic. May 14, 2015. (Accessed 21 Mar 2017.) http://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/expert-answers/vldl-cholesterol/FAQ-20058275 We’ll come back to this a little later, but for now: large and fluffy is good; that’s what you want. Small and sticky is not, for reasons we’ll explain later and because VLDL promotes inflammation in its own right. Oh, and standard cholesterol tests can’t differentiate between the different types of LDL. Big whoops!
Essentially, the problems associated with cholesterol are ones of type and balance, not presence and amount. Forcing the body to throw cholesterol levels out of balance in an attempt to force a global LDL number ever downward, by definition, then, must be an exercise in futility. And we see this in the unchanged mortality numbers revealed in the evolocumab study.
There is a raging debate in the medical community as to the wisdom of forcing cholesterol levels ever lower.
And make no mistake, this opinion is not uniquely mine. You may not hear about it much, but there is a raging debate going on in the medical community as to the wisdom of forcing cholesterol levels ever lower. So, in case it’s not clear, let me clearly restate what the study exposed.
By adding evolocumab to the standard statin regimen, researchers were able to force cholesterol levels to astonishingly low levels. And although doing so may have reduced the “number of cardiovascular incidents,” it made not one whit of difference when it came to mortality rates and hospitalizations–not one whit.
So Why Do Statin Drugs and Evolocumab Lower the Incidence of Cardiovascular Events?
As I’ve explained in previous newsletters, the real culprits behind heart disease are not cholesterol, but excess acidity in the muscle tissue surrounding your arteries and in the arterial walls and systemic inflammation throughout the arterial system. Cholesterol is primarily part of the patching system used to cover over damage to the arterial walls. For the most part, cholesterol is merely guilty of being found at the scene of the crime. You have inflammation and acidity damaging arterial tissue and cholesterol constantly repairing that damage by adding ever more cement-like patches to the arterial walls. This results in a progressive hardening of the arteries and a progressive narrowing of the arterial opening through which your blood flows.
And this is where cholesterol comes into play.
VLDL cholesterol is sticky and causes blood cells to clump together and “thicken’ the blood. As your VLDL numbers climb, your blood steadily thickens, and thick, sticky blood has a harder time passing through narrowed arterial openings. And that’s why higher levels of VLDL (but not fluffy LDL) leads to more cardiovascular events. (But again, remember, standard methods of measurement cannot differentiate between VLDL and LDL. As for as the numbers are concerned, it’s all just LDL.) Lowering overall LDL levels, then, will reduce the number of events, but because lowering cholesterol levels doesn’t’ address the underlying problems–inflammation and damage to the arterial walls–it really doesn’t make much difference when to comes to mortality rates. If you want to lower mortality rates, you have to address the underlying issues.
Now, here’s another surprise. A diet high in saturated fat mainly boosts the numbers of large LDL particles, while a low-fat diet high in carbohydrates increases the smaller forms, the problematic VLDL. Unfortunately, statin drugs and evolocumab neither differentiate nor modulate the size of LDL particles. Nor do they reduce systemic inflammation or ameliorate tissue damage in the arterial walls. All they do is drive the numbers for all types of LDL cholesterol down, ever down–with the consequences we’ve already talked about.
Arterial damage is a better predictor of both the incidence of cardiovascular events and mortality than cholesterol.
Conclusion–What You Can Do
 As we’ve discussed, arterial damage is a better predictor of both the incidence of cardiovascular events and mortality than cholesterol. According to the theory, your body produces arterial plaque in response to arterial damage. Excessive plaque build-up, and the concomitant hardening and narrowing of the arteries, is the result of excessive damage, scarring, and inflammation, in the arterial walls–and the resulting plaque patches. Addressing the underlying issues associated with arterial damage, then, is the way to go. So, what specifically causes damage or inflammation to the arterial walls? Well, among other things:
As we’ve discussed, arterial damage is a better predictor of both the incidence of cardiovascular events and mortality than cholesterol. According to the theory, your body produces arterial plaque in response to arterial damage. Excessive plaque build-up, and the concomitant hardening and narrowing of the arteries, is the result of excessive damage, scarring, and inflammation, in the arterial walls–and the resulting plaque patches. Addressing the underlying issues associated with arterial damage, then, is the way to go. So, what specifically causes damage or inflammation to the arterial walls? Well, among other things:
- High homocysteine levels. Homocysteine is an amino acid produced as a normal byproduct of the breakdown of methionine (from proteins). Methionine is an essential amino acid acquired mostly from eating meat. Methionine is only a problem when it’s broken down. Homocysteine, the byproduct of that breakdown, generates superoxide and hydrogen peroxide, both of which have been linked to damage of the endothelial lining of arterial vessels. Studies have shown that too much homocysteine in the blood is related to a higher risk of coronary heart disease, stroke, and peripheral vascular disease.13 Ellen K Hoogeveen, Pieter J. Kostense, Pieter J. Beks, Coen D. A. Stehouwer. “Hyperhomocysteinemia Is Associated With an Increased Risk of Cardiovascular Disease, Especially in Non–Insulin-Dependent Diabetes Mellitus A Population-Based Study.” Arteriosclerosis Thrombosis and Vascular Biology 18(1):133-8. http://www.researchgate.net/profile/Ellen_Hoogeveen2/publication/13785930_Hyperhomocysteinemia_Is_Associated_With_an_Increased_Risk_of_Cardiovascular_Disease_Especially_in_Non-Insulin-Dependent_Diabetes_Mellitus_A_Population-Based_Study/links/02e7e539f1612d8633000000/Hyperhomocysteinemia-Is-Associated-With-an-Increased-Risk-of-Cardiovascular-Disease-Especially-in-Non-Insulin-Dependent-Diabetes-Mellitus-A-Population-Based-Study.pdf
- Too much Omega-6 fatty acid in the diet. The body converts linoleic acid, the primary fatty acid found in bottled vegetable oil, to arachidonic acid. The Cox-2 enzyme then converts the arachidonic acid to the hormone-like prostaglandin E2 (PGE2) and to the cytokines interleukin-1 (IL-1), interleukin-6 (IL-6), and tumor necrosis factor alpha (TNFa), all of which promote inflammation in the body in general, and in the arterial walls in particular. And the problem doesn’t stop there. The more polyunsaturated fats you eat (just like your doctor tells you to do), the higher your NEFA levels climb. NEFAs (non-esterified fatty acids) in the blood are a build-up of excess omega-6 fats in the body, which are caused by eating an overabundance of polyunsaturated fats such as corn, peanut, sunflower, and safflower oils–in other words, virtually every single bottled vegetable oil and processed food you buy in the supermarket except olive oil. NEFA concentration is an independent risk factor for heart attacks and sudden death.
- Eating high levels of meats and animal fat from grain fattened animals saturates the body with large amounts arachidonic acid and high levels of NEFAs. As a point of interest, the high levels of arachidonic acid found in most commercial meat are accumulated from the conversion of Omega-6 fatty acids present in the grains used to fatten them, especially corn. Only minimal levels of arachidonic acid, on the other hand, are found in range-fed beef. In other words, organic, grass-fed beef doesn’t present these problems and is far healthier for you than the more common grain-fed variety.
- High acid diets. Diets high in meat, sugar, grain, and starch raise acid levels in body tissue — thereby making it difficult for the body to clear the lactic acid that builds up in muscle tissue from normal muscle activity. This is a particular problem for arteries since the arterial wall contains muscle tissue (veins do not) so that the arteries can be contracted to even out blood pressure when changing position (from lying down to suddenly standing up, for example). The problem is that when the acid doesn’t clear from the muscle tissue in the arterial walls, it eventually irritates, inflames, and scars the tissue in the arterial walls. Plaque then forms to patch over this damaged tissue.
- High levels of circulating immune complexes in the blood. Circulating immune complexes (CICs) are created when you eat complex proteins (usually from wheat, corn, and dairy) that cannot be digested thoroughly. They make their way into the bloodstream, where they are treated as allergens by the body and combined with antibodies, thus forming CICs. When the number of CICs climbs beyond the ability of the body to eliminate them all, they are deposited in the body’s soft tissue, including the arterial walls, thereby triggering attacks by the body’s immune system, which results in inflammation of the surrounding soft tissue–which can include the arterial walls.
- Inflammation in general. C-reactive protein (CRP) is an inflammatory marker — a substance that the liver releases in response to inflammation somewhere in the body. Studies indicate that men with high levels of CRP have triple the risk of heart attack and double the risk of stroke compared to men with lower CRP levels. In women, studies have shown that elevated levels of CRP may increase the risk of a heart attack by as much as seven times. The statin medicines (Advicor, Lescol, Lipitor, Mevacor, Pravachol and Zocor), in addition to lowering cholesterol, reduce levels of CRP. This may be more significant in accounting for the ability of these drugs to statistically lower the incidence of heart disease than the role these drugs play in lowering cholesterols. Then again, arginine, Co-Q 10, glutamine, boswellin, and curcumin can all lower CRP levels as well–naturally.
Solutions to Lower Cholesterol Levels
 As we’ve discussed, the cholesterol theory of heart disease has many holes in it, but that said, there are reasons you might want to lower high cholesterol levels into the normal range. So, how do you do that naturally?
As we’ve discussed, the cholesterol theory of heart disease has many holes in it, but that said, there are reasons you might want to lower high cholesterol levels into the normal range. So, how do you do that naturally?
- Avoid manmade trans fatty acids like the plague. Trans fat is finally considered by many doctors to be the worst type of fat you can eat. Unlike other dietary fats, trans fat–also called trans-fatty acids–both raises your LDL cholesterol and lowers your HDL cholesterol. In addition, trans fats play a major role in accelerating atherosclerosis by promoting inflammation and oxidative stress.14 Monguchi T, Haa T, Hasokawa M, et al. “Excessive intake of trans fatty acid accelerates atherosclerosis through promoting inflammation and oxidative stress in a mouse model of hyperlipidemia.” J Cardiol. 2017 Feb 18. pii: S0914-5087(17)30015-1. http://www.ncbi.nlm.nih.gov/pubmed/28254384 Quite simply, partially hydrogenated oils (the trans fatty acids) are the number one killer in the modern diet. Note: naturally occurring trans fats are generally not a problem.
- Optimize the liver. Do a periodic liver flush that includes the use of lipotropic herbs such as dandelion root to flush accumulated fats and cholesterol from the liver and gallbladder–thus freeing up the liver to better perform its job of clearing excess cholesterol from the bloodstream.
- Lower homocysteine levels. While there is a considerable amount we do not know about homocysteine, we do know how to use nutritional supplements to reduce homocysteine levels. This is done through three independent routes: (1) using folic acid with vitamin B-12, (2) using trimethylglycine (TMG), and (3) through B-6. The first two work through a process called methylation, and the B-6 through transsulfuration. Such a combined approach can normalize homocysteine in 95% of the people studied. (Look for a mix that contains approximately 50 mg of B6, 500 mcg of B12, 800 mcg of folic acid, and 500 mg of TMG)
- Optimize Omega-6 to Omega-3 ratios by eliminating bottled vegetable oils found in your supermarket, except for olive oil, and supplementing with fish oil, krill oil, and flax seed oil, which are high in Omega-3 fatty acids. Much of the problem with inflammatory disorders actually stems from a lopsided imbalance in the dietary intake of the omega-6 and omega-3 fatty acids and the resulting cascade in pro-inflammatory activity. The ideal ratio is roughly 1 to 1; however, over the past 40 years, people from industrialized countries have replaced much of their dietary saturated fat (on the mistaken advice of their doctors and the media) with vegetable oil omega-6 fatty acids. Ratios of 20 to 1 and 30 to 1 are now not uncommon. From a biochemical standpoint, this sets the stage for major arterial inflammation.
- A good antioxidant formula that contains OPCs, can help repair damage to arterial walls.
- Systemic Proteolytic Enzymes. This is one of the most important things you can do. The regular use of proteolytic enzymes can help eliminate CICs from the body, reduce overall inflammation, dissolve accumulated plaque, declump blood cells and optimize the flow of blood, and repair arterial scar tissue. Although the evidence is purely anecdotal at the moment, we have seen extraordinary results using detox levels of this formula.
The bottom line is that unless you’re suffering from a genetic disorder that is pushing your cholesterol numbers up to insanely high levels, you probably don’t want to think about spending $174,000 dollars a year for evolocumab. There are better ways to go.

References
| ↑1 | American College of Cardiology. “Evolocumab significantly reduces risk of cardiovascular events.” ScienceDaily. March 17, 2017. (Accessed 22 Mar 2017.) http://www.sciencedaily.com/releases/2017/03/170317132012.htm |
|---|---|
| ↑2 | Bazian. “New drug shows promise in preventing heart attacks.” NHS Choices. March 20, 2017. (Accessed 22 Mar 2017.) http://www.nhs.uk/news/2017/03March/Pages/New-drug-shows-promise-in-preventing-heart-attacks.aspx |
| ↑3 | Deborah Brauser. “Evolocumab Added to Statins Cuts CV Events in FOURIER Trial.” Medscape. March 17, 2017. (Accessed 22 Mar 2017.) http://www.medscape.com/viewarticle/877348 |
| ↑4 | Sabatine MS, Giugliano RP, Keech AC, et al. “Evolocumab and Clinical Outcomes in Patients with Cardiovascular Disease.” NEJM. March 17, 2017. http://www.nejm.org/doi/full/10.1056/NEJMoa1615664#t=article |
| ↑5 | GINA KOLATA. “Cholesterol-Slashing Drug Can Protect High-Risk Heart Patients, Study Finds.” New York Times. MARCH 17, 2017. (Accessed 20 March 2017). http://www.nytimes.com/2017/03/17/health/cholesterol-drugs-repatha-amgen-pcsk9-inhibitors.html |
| ↑6 | http://en.wikipedia.org/wiki/Blue_Screen_of_Death |
| ↑7 | Yuki A, Otsuka R, Kozakai R, et al. “Relationship between low free testosterone levels and loss of muscle mass.” Sci Rep. 2013;3:1818. http://www.ncbi.nlm.nih.gov/pubmed/23660939 |
| ↑8 | Steegmans PH, Hoes AW, Bak AA, et al. “Higher Prevalence of Depressive Symptoms in Middle-Aged Men With Low Serum Cholesterol Levels.” Psychosomatic Medicine: March/April 2000 – Volume 62 – Issue 2 – pp 205-211. http://journals.lww.com/psychosomaticmedicine/Abstract/2000/03000/Higher_Prevalence_of_Depressive_Symptoms_in.9.aspx |
| ↑9 | CAROLINE WELLBERY. “Low Cholesterol Levels Associated with Increased Mortality.” Am Fam Physician. 2005 Nov 1;72(9):1859-1860. http://www.aafp.org/afp/2005/1101/p1859.html |
| ↑10 | Wu S, Ding Y, Wu F, Xie G, Hou J, Mao P. “Serum lipid levels and suicidality: a meta-analysis of 65 epidemiological studies.” J Psychiatry Neurosci. 2016 Jan;41(1):56-69. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4688029/ |
| ↑11 | Oh J, Kim TS. “Serum lipid levels in depression and suicidality: The Korea National Health and Nutrition Examination Survey (KNHANES) 2014.” J Affect Disord. 2017 Apr 15;213:51-58. http://www.ncbi.nlm.nih.gov/pubmed/28189965 |
| ↑12 | Francisco Lopez-Jimenez. “VLDL cholesterol: Is it harmful?” Mayo Clinic. May 14, 2015. (Accessed 21 Mar 2017.) http://www.mayoclinic.org/diseases-conditions/high-blood-cholesterol/expert-answers/vldl-cholesterol/FAQ-20058275 |
| ↑13 | Ellen K Hoogeveen, Pieter J. Kostense, Pieter J. Beks, Coen D. A. Stehouwer. “Hyperhomocysteinemia Is Associated With an Increased Risk of Cardiovascular Disease, Especially in Non–Insulin-Dependent Diabetes Mellitus A Population-Based Study.” Arteriosclerosis Thrombosis and Vascular Biology 18(1):133-8. http://www.researchgate.net/profile/Ellen_Hoogeveen2/publication/13785930_Hyperhomocysteinemia_Is_Associated_With_an_Increased_Risk_of_Cardiovascular_Disease_Especially_in_Non-Insulin-Dependent_Diabetes_Mellitus_A_Population-Based_Study/links/02e7e539f1612d8633000000/Hyperhomocysteinemia-Is-Associated-With-an-Increased-Risk-of-Cardiovascular-Disease-Especially-in-Non-Insulin-Dependent-Diabetes-Mellitus-A-Population-Based-Study.pdf |
| ↑14 | Monguchi T, Haa T, Hasokawa M, et al. “Excessive intake of trans fatty acid accelerates atherosclerosis through promoting inflammation and oxidative stress in a mouse model of hyperlipidemia.” J Cardiol. 2017 Feb 18. pii: S0914-5087(17)30015-1. http://www.ncbi.nlm.nih.gov/pubmed/28254384 |











This article contains very
This article contains very useful information. I now know that in order to free my arteries from plague, and improve blood flow, I need to get hold of Systematic proteolytic enzymes.
Can any one out there advise me where to buy these enzymes?
All our recommended formulas
All our recommended formulas are listed under the “Products” tab at the top of the page. For this one, you can find it here: http://www.baselinenutritionals.com/products/all-products/phi-zymes-90.php
hi john,another fascinating
hi john,another fascinating article.i was wondering what your take on the unified theory of heart disease by pauling and rath that lpa acts as asurrogate for low vitamin c and hardens weak blood vessels.
A quick question. In this
A quick question. In this article you state “naturally occurring trans fats are generally not a problem”. What “naturally occurring trans fats”? I always believed that there are no trans fats in nature since they are formed by the bubbling of hydrogen into oils.
Artificial trans fats are
Artificial trans fats are major contributors to cancer, heart disease, and diabetes and have no place in your diet if you wish to be healthy. But naturally occurring trans fats can be healthy. Conjugated linoleic acid (CLA) is both a trans-fatty acid and a cis-fatty acid that has major health benefits. Studies have indicated it is a potent cancer fighter across a wide variety of tumors, can lower LDL cholesterol levels, prevent bone loss and atherosclerosis, and is actually brain protective. Natural trans fats are created in the stomachs of ruminant animals such as cattle, sheep, goats, etc. and make their way into the fat stores of the animals. Therefore, the milk fat and the fat within the meat of these animals can provide natural healthy trans fats (best in grass-fed organic versions). As it turns out, grazing animals have 3-5 times more CLA than grain fattened animals — providing yet one more reason for consuming grass fed animal products. As a side note, the breast milk of mothers who consume foods high in CLA is likewise high in CLA, providing tremendous health benefits for the baby.
Jon,
Jon,
This article is long and good but
with no conclusions.
How low can it go without being armful?
Do you know?
If so, please tell me.
Good letter,
Best regards,
Yvon
Wrong question. The question
Wrong question. The question you want to ask is: what’s a health level? Now, to answer that question, let’s take a look at the country that has the lowest incidence of cardiovascular disease: South Korea. And what is their average cholesterol profile? It turns out that South Koreans average a total cholesterol reading in the mid 180’s. In other words, it would appear that you don’t need to go any lower than that for optimum heart health—assuming all the rest of your markers (HDL/LDL ratio, triglycerides, NEFA’s, blood cell clumping, systemic inflammation, tissue acidity, etc.) are in good shape.
A very very good read. I have
A very very good read. I have never heard of the concept of the muscle and acid build up in the muscle of the artery wall as an instigator of damage to the wall. I have heard of high blood pressure in the artery especially at the branching points as being the main culprit. I have heard of small particle LDL and of oxidized oil or oil that is off or damaged by heat as I understand that their are receptors on the artery wall that will attract that oil and I have heard of teeth bacteria lodging themselves on the artery wall so this is a new one to me and of interest. Still a heart attack can come from a stressful situation as the main instigator. I am surprised that you are not on some advisory board or attached as a bridging voice to govt to make some insightful analysis as to the role of alternative health and modern medicine as neither are ever going to go away in the long or short term and must somehow get along together or live unhappily married. Just of interest I remember getting a letter from a vegetarian mob( renegade health) that they managed to cite some research showing a graph plotting LDL cholesterol against heart attacks, if I remember correctly, there was a point that they claimed were if you got the LDL below a certain point there were no cardiac events. Good in theory I would suggest. Can you have low or normal blood pressure and significant arterial plaques or high blood pressure and no significant plaques?
Yes, high blood pressure has
Yes, high blood pressure has been identified as a risk factor in the development of arterial plaque, but not the definitive risk factor. On the other hand, the build-up of arterial plaque is a definitive risk factor for high blood pressure. And yes, it’s quite possible to have a cardiac event with extremely low LDL. In fact, that was demonstrated in the evolocumab study, cited above, which explored what happens when you take LDL down to never before seen low levels. Yes, there were fewer cardiac events (a very modest improvement)—but fewer is not none. And more importantly, there was no change in mortality rates.