The American Cancer Society (ACS), the Centers for Disease Control and Prevention (CDC), the National Cancer Institute (NCI), and the North American Association of Central Cancer Registries (NAACCR) collaborate to provide annual updates on cancer occurrence and trends in the United States. On May 22nd, they released their latest Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics.1 Kathleen A. Cronin, Andrew J. Lake, Susan Scott, et al. “Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics.” Cancer. 22 May 2018. http://onlinelibrary.wiley.com/doi/full/10.1002/cncr.31551
Not surprisingly, they patted themselves on the back. As NCI Director Ned Sharpless, M.D said, “This year’s report is an encouraging indicator of progress we’re making in cancer research. As overall death rates continue to decline for all major racial and ethnic groups in the United States, it’s clear that interventions are having an impact. The report also highlights areas where more work is needed. With steadfast commitment to patients and their families, we will be able to lower the mortality rates faster and improve the lives of those affected by cancer.”
So, as always, the question of the day remains: is such self-congratulations warranted? And the answer is: yes, some progress has been made, but not as much as is claimed. But on a happier note, medical gains against cancer are likely to be faster and more pronounced moving forward.
Summary of the Annual Report
Note: the report explored data for both cancer incidence and mortality. The incidence data for the report was obtained from the CDC‐ and NCI‐funded population‐based cancer registry. Data on deaths from cancer was obtained from the National Center for Health Statistics National Vital Statistics System. According to the report:
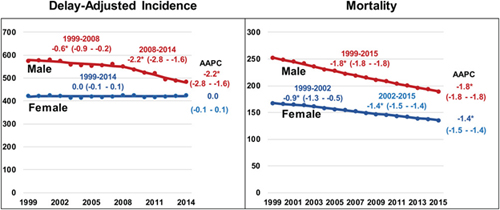
- Overall cancer mortality rates decreased by 1.8% per year among men and by 1.4% per year among women from 1999 to 2015.
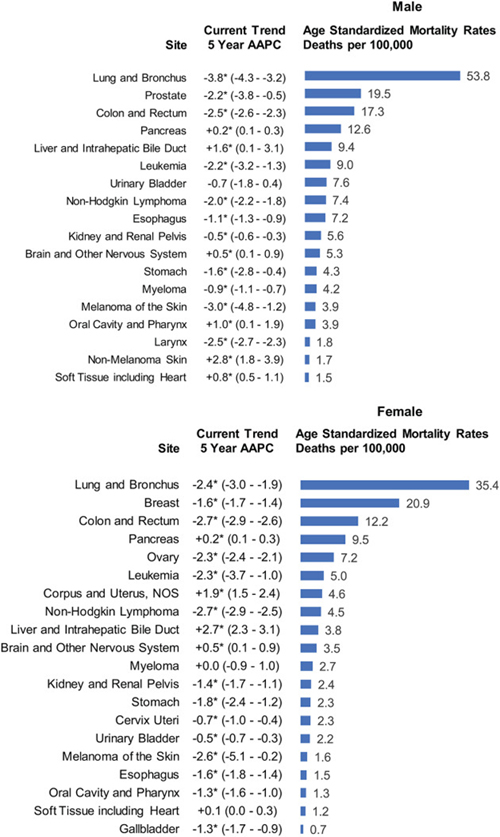
- Among men, death rates (2011‐2015) decreased for 11 of the 18 most common types.
- Among women, death rates declined for 14 of the 20 most common cancers.
- Among children, overall cancer death rates decreased by 1.5% per year from 2011 to 2015.
- Death rates decreased for cancer sites, including lung and bronchus (men and women), colorectal (men and women), female breast, and prostate.
- Death rates increased for cancers of the liver (men and women); pancreas (men and women); brain and other nervous system (men and women); oral cavity and pharynx (men only); soft tissue, including heart (men only); nonmelanoma skin (men only); and uterus.
- Incidence and death rates were higher among men than among women for all racial and ethnic groups.
- For all cancer sites combined, black men and white women had the highest incidence rates compared with other racial groups, and black men and black women had the highest death rates compared with other racial groups.
- Non‐Hispanic men and women had higher incidence and mortality rates than those of Hispanic ethnicity.
- Five‐year survival for cases diagnosed from 2007 through 2013 ranged from 100% (stage I) to 26.5% (stage IV) for female breast cancer, from 88.1% (stage I) to 12.6% (stage IV) for colorectal cancer, from 55.1% (stage I) to 4.2% (stage IV) for lung and bronchus cancer, and from 99.5% (stage I) to 16% (stage IV) for melanoma of the skin.
In summary, for all types of cancer combined, cancer incidence rates decreased among men but were stable among women, with both incidence and death rates higher in men than in women in every racial and ethnic group. Also, there continue to be significant declines in cancer death rates among both men and women. That said, progress in reducing cancer mortality has not occurred for all types of cancer. Increases in death rates for several cancers continue to cause concern. Researchers suggest that the increase in liver cancer death rates is related to the high prevalence of hepatitis C virus infection among Baby Boomers, as well as to the high prevalence of obesity in the United States. Obesity is also thought to have contributed to the increase in death rates from cancers of the uterus and pancreas. The recent increase in oral cavity and pharynx cancer death rates among white men is thought to be associated with human papillomavirus infection.
According to the Director of the National Cancer Institute, Ned Sharpless, M.D., “This year’s report is an encouraging indicator of progress we’re making in cancer research. As overall death rates continue to decline for all major racial and ethnic groups in the United States, it’s clear that interventions are having an impact.”
Finally, the report also describes five-year survival during 2007-2013 by cancer stage at diagnosis for four of the most common cancers–female breast cancer, colorectal cancer, lung and bronchus cancer, and melanoma of the skin. While five-year survival is high for early-stage disease for breast cancer, colorectal cancer, and melanoma, survival remains low for all stages of lung cancer, ranging from 55 percent for Stage I to 4 percent for Stage IV.
“This report underscores that if cancer is caught early, when it has the best chance of being treated, patients can live longer,” said CDC Director Robert R. Redfield, M.D. “Early detection and timely, quality treatment are keys to saving lives.”
Prostate Cancer
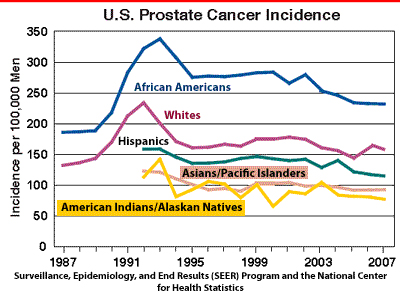
 In a companion study, researchers explored prostate cancer trends in more detail.2 Negoita S, Feuer EJ, Mariotto A1, Cronin KA, et al. “Annual Report to the Nation on the Status of Cancer, part II: Recent changes in prostate cancer trends and disease characteristics.” Cancer. 2018 May 22. http://onlinelibrary.wiley.com/doi/full/10.1002/cncr.31549 They found that overall prostate cancer incidence rates declined an average of 6.5 percent each year between 2007 and 2014. However, the incidence of “distant disease”–that is, of cancer that has spread from the original tumor to other parts of the body–increased from a low rate of 7.8 new cases per 100,000 in 2010 to 9.2 new cases per 100,000 in 2014. Furthermore, after two decades of decline between 1993 and 2013, prostate cancer mortality leveled off between 2013 and 2015.
In a companion study, researchers explored prostate cancer trends in more detail.2 Negoita S, Feuer EJ, Mariotto A1, Cronin KA, et al. “Annual Report to the Nation on the Status of Cancer, part II: Recent changes in prostate cancer trends and disease characteristics.” Cancer. 2018 May 22. http://onlinelibrary.wiley.com/doi/full/10.1002/cncr.31549 They found that overall prostate cancer incidence rates declined an average of 6.5 percent each year between 2007 and 2014. However, the incidence of “distant disease”–that is, of cancer that has spread from the original tumor to other parts of the body–increased from a low rate of 7.8 new cases per 100,000 in 2010 to 9.2 new cases per 100,000 in 2014. Furthermore, after two decades of decline between 1993 and 2013, prostate cancer mortality leveled off between 2013 and 2015.
This study also reports a decline in prostate-specific antigen (PSA) screening based on a series of national surveys. The reported decline in screening occurred between the 2010 and 2013 surveys for men between 50 and 74 years of age, and after the 2008 survey for men age 75 and older.
According to Serban Negoita, lead author of the study, “The increase in late-stage disease and the flattening of the mortality trend occurred contemporaneously with the observed decrease in PSA screening in the population. Although suggestive, this observation does not demonstrate that one caused the other, as there are many factors that contribute to incidence and mortality, such as improvements in staging and treating cancer. Additional research is needed to get a more comprehensive understanding of the recent trends and the possible relationship with PSA screening, as well as the relationship with other factors that may be associated with these trends.”
Yes, but
The report is enthusiastic about two things: the incidence of cancer is down and mortality is down–particularly the five year survival rate. Again, to quote Robert Redfield, “This report underscores that if cancer is caught early, when it has the best chance of being treated, patients can live longer.” So, let’s take a look at those two claims.
The Incidence of Cancer is Down
So, what’s my problem with this claim? Quite simply: incidence may be down, but what does medical care have to do with it? It’s not like doctors are giving people a cancer vaccine that prevents cancer. No, that medical care has little to do it. On the other hand, doctors are no longer doing things that promote a higher incidence of cancer. I’m talking about:
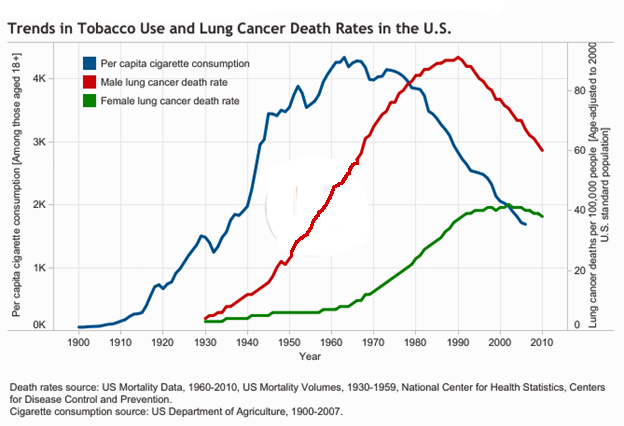
- The reduction in cigarette smoking. This is the major reason that both lung cancer incidence and mortality rates have declined. And let’s not forget that not only does smoking increase the risk for lung cancer, it’s also a risk factor for cancers of the: Mouth, Larynx (voice box), Pharynx (throat), Esophagus (swallowing tube), Kidney, Cervix, Liver, Bladder, Pancreas, Stomach, Colon/rectum, and Myeloid leukemia3 “Health Risks of Smoking Tobacco.” ACS. (Accessed 12 Jun 2018.) http://www.cancer.org/cancer/cancer-causes/tobacco-and-cancer/health-risks-of-smoking-tobacco.html –oh, and prostate cancer.4 Freedland SJ. Smoking and Death From Prostate Cancer. JAMA Oncol. Published online May 24, 2018. http://jamanetwork.com/journals/jamaoncology/article-abstract/2682184 A recent meta-analysis showed that smokers are 24% more likely than nonsmokers to die from prostate cancer. So, we’re talking about reducing a whole lot of cancer incidence and mortality simply from the reduction in smoking in the US. But can doctors claim credit for the reduction–especially when they played a major role in promoting cigarette smoking in the first place?5 Devra Davis. The Secret History of the War on Cancer. NY, New York: Basic Books, 2007.
- In case you’re too young to remember, the Journal of the American Medical Association ran ads for cigarettes from 1933-1953 and published position papers promoting the virtues of cigarette smoking. Yes, they really did that.6 “THE ADVERTISING OF CIGARETTES.” JAMA. 1948;138(9):652-653. http://jamanetwork.com/journals/jama/article-abstract/302011
- Then there’s breast cancer, the second leading cancer for women after lung cancer. It has become clear that long-term use (several years or more) of hormone replacement therapy after menopause increases the risk of both breast cancer7 Chlebowski, Rowan T., Kuller, Lewis H., Prentice, Ross L., et al. “Breast Cancer after Use of Estrogen plus Progestin in Postmenopausal Women.” N Engl J Med Volume 360, Number 6, pages 573-587, February 5, 2009. http://www.nejm.org/doi/full/10.1056/NEJMoa0807684 and ovarian cancer,8 Karpasea-Jones, Joanna. “Hormone Replacement Therapy May Cause 5 Percent of Ovarian Cancer.” Empowher. 10 October 2012. (Accessed 14 June 2018.) http://www.empowher.com/cancer/content/hormone-replacement-therapy-may-cause-5-percent-ovarian-cancer as well as the risk of heart disease, blood clots, and strokes. (Note: five years after stopping HRT, the breast cancer risk appears to drop back to normal.) Additionally, studies have found that women now using birth control pills have a greater risk of breast cancer than women who have never used them.9 “Oral Contraceptives and Cancer Risk.” NCI. Reviewed 22 Feb 2018. (Accessed 14 Jun 2018.) http://www.cancer.gov/about-cancer/causes-prevention/risk/hormones/oral-contraceptives-fact-sheet (After 10 years of non-use, the risk goes away.) Some experts believe U.S. breast cancer rates dropped sharply in 2003 because many women suddenly stopped menopausal hormone10 “Number of prescriptions for hormone replacement therapy (HRT) drugs among adult U.S. women from 2001 to 2008 (in millions)” statista. (Accessed 14 Jun 2018.) http://www.statista.com/statistics/305412/prescriptions-for-hormone-replacement-therapy-drugs-us-women/ use after disturbing results from the Women’s Health Initiative study were released. So once again, we have to ask the question: do doctors get to claim credit for a reduction in breast cancer rates simply by reducing the number of prescriptions they were writing for the HRT–those same prescriptions that were causing much of the cancer in the first place?
- And we see the same thing with prostate cancer. Looking at the incidence rates, we see rates rise dramatically in the late ‘80s when PSA testing came into wide use. But since the early ‘90s, incidence has been steadily declining. What could have been responsible? Well, when we look at the trend in tobacco use chart that we saw earlier, we can see that the decline in incidence perfectly aligns with the years men started to quit smoking in large numbers. So once again, it’s hard to credit the medical community for the decline in the incidence of prostate cancer.
The bottom line is that if the medical community wants to take credit for the downward trend in cancer incidence, considering they had nothing to do with it, then we should expect them to take the blame for the surge in suicide rates to the highest levels in 30 years11 Sally C. Curtin, Margaret Warner, and Holly Hedegaard. “Increase in Suicide in the United States, 1999–2014.” CDC. NCHS Data Brief No. 241, April 2016. http://www.cdc.gov/nchs/products/databriefs/db241.htm –even though they have no direct connection with that situation. Fair is fair.
People Are Living Longer with Cancer
And then the medical community claims that people are living longer–largely thanks to early detection and improved treatments.
Well, if you want to be snarky about it:
- Even if the treatment makes no difference and you die at exactly the same time as you would have without the treatment
- But you detected the cancer 1-2 years earlier
- Then statistically, it will look like you lived 1-2 years longer–even though you didn’t
And yes, there’s some truth to our little syllogism. But to be fair, there have been some major advances in cancer treatment that have indeed extended life beyond the extra innings that result from earlier detection.
Surgery
Thanks to changes in medical thinking (no more radical mastectomies) plus the advent of laparoscopic and micro surgery, cancer surgery is much less brutal and disfiguring than it was in years past. And yes, if the cancer has not metastasized and you remove all the offending tumor, then yes, the cancer is gone. But if you don’t remove the trigger (e.g. radon gas in your house, carcinogens in your diet, menopausal HRT, etc.), then you haven’t really resolved the issue so the cancer is likely to return anyway.
Radiation
As with surgery, the advent of computerized targeting has allowed radiation therapy to be much more precise–that is, to do a much better job at destroying all the cancer (assuming it hasn’t metastasized), while at the same time minimizing damage to nearby healthy tissue. But radiation is still radiation, and it still has long-term impact on the body. And as with surgery, since it doesn’t address the underlying trigger, there’s the likelihood of the cancer returning anyway.
Chemotherapy
On the positive side, doctors have learned to be much more targeted with chemo–to identify which drugs work best with which cancers and to precisely optimize dosage to minimize harm to healthy cells. But you still have a problem. As I’ve explained in other newsletters, even treatments that are 99.9% effective in getting rid of the cancer cells in your body are still likely to fail. They simply leave too many viable cancer cells behind–potentially millions of surviving cancer cells, actually. To consider yourself cured, or at least in long-term remission, you actually have to destroy 99.9999999999% of all the cancer cells in your body. And that means that no matter how precise you are when it comes to dosing, you have to use a level of chemotherapy that is likely to be harmful to healthy tissue–or even fatal when it comes to the more serious cancers–if you’re looking for a successful outcome. That said, there are advances in chemotherapy that are being tested now that allow for those higher doses while at the same time protecting the body from any harm…or even any side effects, for that matter.
Virotherapy
Virotherapy can, for some cancers and some patients, be an effective cancer treatment. It involves injecting the patient with a special virus capable of finding and destroying malignant tumor cells. Viruses, as we know, can travel in the bloodstream and reach every area of the body, thus reaching every malignant cell wherever it might be hiding. Theoretically, virotherapy destroys tumor cells selectively without affecting the healthy cells of the body. It also stimulates the body’s natural defense mechanisms by activating the immune system, which is often suppressed by other treatment methods. And finally, it can be used against tumors that don’t respond well to radiation or chemotherapy, such as melanomas.
The greatest challenge in virotherapy, however, is making sure that viruses reach all tumor tissue at sufficient levels to pass from blood vessels into the tumor, replicate in tumor cells to create infectious centers, which then expand outwards and merge to destroy the tumor or perform effective tumor debulking. This requires constantly increasing the dose of the virus used for injection until it’s sufficient to cross what is known as “the threshold dose.”
But virotherapy is an emerging field, and the medical community needs to work through some major obstacles before it can become a mainstream treatment:
- A virus is a virus, which means your body will treat it as an invader, not just by attacking it with immune cells, but also by sequestering the virus in the liver and spleen. That’s not useful if your cancer is located someplace else.
- As we just mentioned, your immune system will try to neutralize the virus using serum immune factors.
- The virus needs to be “modified” to “selectively” bind to tumor tissue.
- Along with the introduction of the virus, you need to selectively increase the permeability of tumor blood vessels to allow the virus to enter the tumor in massive numbers while avoiding systemic inflammation in the rest of the body.
It’s early days.
Cancer Immunotherapy (Immuno-Oncology)
This is virtually the same deal as virotherapy, but instead of using a virus, it uses your own immune system to attack the cancer. Theoretically, this should be a more “natural” approach since your immune system is already designed to seek out and destroy cancerous cells. And unlike with virotherapy, you don’t have to worry about immune cells attacking themselves or being sequestered in the liver and spleen. On the other hand, it may require some extra training for those immune cells to identify the cancer cells that have learned how to hide from your immune system.
The promise of Immuno-Oncology (IO) is based on the knowledge that the immune system is constantly searching for, assessing, and eliminating foreign particles from the body.12 Melero I et al. “Clinical development of immunostimulatory monoclonal antibodies and opportunities for combination.” Clin Cancer Res 2013; 19: 997-100. http://clincancerres.aacrjournals.org/content/clincanres/19/5/997.full.pdf , 13 Finn O. “Immuno-oncology: understanding the function and dysfunction of the immune system in cancer.” Annals of Oncology 23 (Supplement 8): viii6-viii9, 2012. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085883/ Yet, sometimes rogue cells slip past this immune surveillance and become cancers.14 Finn By providing the immune system with tools to both unmask tumors and strengthen your body’s ability to attack harmful cells, IO therapies enable the immune system to recognize and respond.15 Melero , 16 Eggermont A and Finn O. “Advances in immuno-oncology.” Annals of Oncology, Volume 23, Issue suppl_8, 1 September 2012: viii5. http://academic.oup.com/annonc/article/23/suppl_8/viii5/185159
The primary problem with Immunotherapy is that it doesn’t work for patients with weak immune systems, which, when you’re dealing with cancer patients, leaves out 70-80% of all patients. The next step for immuno-oncology therapies, then, is to make them effective in those patients by figuring out how to activate T-CD8 cells (killer T cells) that kill tumor cells in those patients whose immune systems are normally too weak to respond.
Gene Editing
Okay, we talked about this in our last newsletter, and several people wrote in to tell us they didn’t like it. But the truth is that although approaches including diet and supplements can protect your DNA from damage and can even alter the ability of damaged genes from expressing themselves and manifesting illness, there is little evidence that any tools in the alternative arsenal can “repair” damaged or faulty DNA. Gene editing theoretically can do that.
Look, the technology isn’t there yet, and there are ethical issues associated with gene manipulation, but the potential is undeniable. Theoretically, one day in the future your doctor will be able to get rid of any cancer you have simply by “editing” the cancer cells in your body out of existence. You don’t need to surgically remove them, burn them, poison them, send a virus after them, or even call up your immune system. It’s more like one day you have cancer cells, and the next day, those same cells are now normal. Cancer gone.
Again, the technology isn’t there yet, but it’s advancing rapidly, and whether we like the idea or not, within most of our lifetimes, this approach will at least start to become a reality.
Conclusion
So, what is the answer to the question of whether or not the medical community’s self-congratulations in terms of cancer is warranted?
- When it comes to reducing the incidence of cancer, the medical community has very little to do with it
- But when it comes to extending life for those with cancer, yes, the medical community has made strides and deserves credit for it–just not quite as much as they claim
On a happier note, medical gains against cancer are likely to be faster and more pronounced moving forward. Look, for years, medical treatments for cancer were almost as harmful as the gains they provided. Pursuing alternative choices was definitely a favorable option. But we may be approaching a tipping point where alternative protocols will still be your best bet for avoiding cancer–but medical treatments may be your best option for getting rid of it if you have it.
With that in mind, there are things you should be doing now to optimize your baseline of health so that you either significantly reduce your chances of getting cancer in the first place (preventing cancer is much easier than getting rid of it), or possibly reversing the cancer on your own by charging up your body to do what it was designed to do. Or, at the very least, put yourself in a much better position to have a positive response to any medical treatment you receive (such as having a strong enough immune system to benefit from cancer immunotherapy)–or in some cases, as things currently stand, just survive the treatment. Think of it as natural health insurance.

References
| ↑1 | Kathleen A. Cronin, Andrew J. Lake, Susan Scott, et al. “Annual Report to the Nation on the Status of Cancer, part I: National cancer statistics.” Cancer. 22 May 2018. http://onlinelibrary.wiley.com/doi/full/10.1002/cncr.31551 |
|---|---|
| ↑2 | Negoita S, Feuer EJ, Mariotto A1, Cronin KA, et al. “Annual Report to the Nation on the Status of Cancer, part II: Recent changes in prostate cancer trends and disease characteristics.” Cancer. 2018 May 22. http://onlinelibrary.wiley.com/doi/full/10.1002/cncr.31549 |
| ↑3 | “Health Risks of Smoking Tobacco.” ACS. (Accessed 12 Jun 2018.) http://www.cancer.org/cancer/cancer-causes/tobacco-and-cancer/health-risks-of-smoking-tobacco.html |
| ↑4 | Freedland SJ. Smoking and Death From Prostate Cancer. JAMA Oncol. Published online May 24, 2018. http://jamanetwork.com/journals/jamaoncology/article-abstract/2682184 |
| ↑5 | Devra Davis. The Secret History of the War on Cancer. NY, New York: Basic Books, 2007. |
| ↑6 | “THE ADVERTISING OF CIGARETTES.” JAMA. 1948;138(9):652-653. http://jamanetwork.com/journals/jama/article-abstract/302011 |
| ↑7 | Chlebowski, Rowan T., Kuller, Lewis H., Prentice, Ross L., et al. “Breast Cancer after Use of Estrogen plus Progestin in Postmenopausal Women.” N Engl J Med Volume 360, Number 6, pages 573-587, February 5, 2009. http://www.nejm.org/doi/full/10.1056/NEJMoa0807684 |
| ↑8 | Karpasea-Jones, Joanna. “Hormone Replacement Therapy May Cause 5 Percent of Ovarian Cancer.” Empowher. 10 October 2012. (Accessed 14 June 2018.) http://www.empowher.com/cancer/content/hormone-replacement-therapy-may-cause-5-percent-ovarian-cancer |
| ↑9 | “Oral Contraceptives and Cancer Risk.” NCI. Reviewed 22 Feb 2018. (Accessed 14 Jun 2018.) http://www.cancer.gov/about-cancer/causes-prevention/risk/hormones/oral-contraceptives-fact-sheet |
| ↑10 | “Number of prescriptions for hormone replacement therapy (HRT) drugs among adult U.S. women from 2001 to 2008 (in millions)” statista. (Accessed 14 Jun 2018.) http://www.statista.com/statistics/305412/prescriptions-for-hormone-replacement-therapy-drugs-us-women/ |
| ↑11 | Sally C. Curtin, Margaret Warner, and Holly Hedegaard. “Increase in Suicide in the United States, 1999–2014.” CDC. NCHS Data Brief No. 241, April 2016. http://www.cdc.gov/nchs/products/databriefs/db241.htm |
| ↑12 | Melero I et al. “Clinical development of immunostimulatory monoclonal antibodies and opportunities for combination.” Clin Cancer Res 2013; 19: 997-100. http://clincancerres.aacrjournals.org/content/clincanres/19/5/997.full.pdf |
| ↑13 | Finn O. “Immuno-oncology: understanding the function and dysfunction of the immune system in cancer.” Annals of Oncology 23 (Supplement 8): viii6-viii9, 2012. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4085883/ |
| ↑14 | Finn |
| ↑15 | Melero |
| ↑16 | Eggermont A and Finn O. “Advances in immuno-oncology.” Annals of Oncology, Volume 23, Issue suppl_8, 1 September 2012: viii5. http://academic.oup.com/annonc/article/23/suppl_8/viii5/185159 |












What basic steps can Jon
What basic steps can Jon Barron outline for consideration by my family and close friends for the “…things you should be doing now to optimize your baseline of health so that you either significantly reduce your chances of getting cancer in the first place (preventing cancer is much easier than getting rid of it), or possibly reversing the cancer on your own by charging up your body to do what it was designed to do.” ?
Thanks!
Hi Jim,
Hi Jim,
Have you read Jon’s book? We have a free download and audio: http://www.jonbarron.org/barron-lessons-from-the-miracle-doctors
I used to work for
I used to work for oncologists many years ago and even back then they knew everything about cancer, from cause, to prevention, and cure. All this was based on the ‘free radical theory of cancer’ an excellent piece of scientific information that was so good the medical industry had it buried because it threatened their cancer treatment profits. Basically the message of that theory was this: you don’t get cancer because your body isn’t making enough chemo drugs – get it?
Makes sense. Why would they
Makes sense. Why would they want to cure or prevent cancer?
It’s a Zillon dollar profit maker! The people at those groups would all be out of jobs!