Well, I was planning a different health newsletter for this issue, but the results of a new study on calcium have just been published, and the media, as might be expected, is going nuts with dramatic headlines.
- Calcium Supplements May Boost Heart Attack Risk
- Dispatch: Have A Heart, Don’t Eat Calcium Supplements
- Study: Calcium May Increase Heart Attack Risk
And it’s hardly surprising that since calcium is one of the world’s favorite dietary supplements — and is added as a “functional” ingredient to everything from margarine to orange juice — attacking its “safety” is going to be just downright confusing to most people and scare the heck out of many of them. And right on cue, the questions have already started pouring into the Baseline of Health Foundation concerning calcium as a natural health alternative. So before it gets out of hand, let me address the calcium issue one more time.
The calcium myth
Although we live in a calcium obsessed society, I’ve never actually been that big a fan of calcium supplementation. Yes, I understand that virtually every health expert in the world has told us to supplement with more and more calcium, and as I mentioned above, it’s one of the hottest dietary supplements and food additives in the world. But the simple truth is: the vast majority of people get more than enough calcium in their diets. In fact, most people get too much. The average American consumes 600 lbs of dairy products a year. That’s almost 2 lbs per day, and yet osteoporosis rates in the United States are among the highest in the world. In fact, several years ago, researchers at Yale University analyzed 34 published studies from 16 different countries and found that the countries with the highest rates of osteoporosis (including the United States, Sweden, and Finland) were those in which people consumed the most meat, milk, and other animal-based foods. The study also showed that African-Americans, who consume, on average, more than 1,000 mg of calcium per day, are nine times more likely to experience hip fractures than are South African blacks, whose daily calcium intake is only about 196 mg. On a nation-by-nation basis, people who consume the most calcium have the weakest bones and the highest rates of osteoporosis.
The interesting thing is that our world-wide obsession with calcium is a relatively new phenomenon. It actually started in the 1950’s under pressure from the American dairy industry. Before then, historically, people didn’t consume much calcium — and had very few problems with osteoporosis. What they did consume was magnesium — almost 5 times as much magnesium as we consume today. Which brings up a key point: the health of our bones depends far more on other factors such as magnesium, boron, vitamin K, and vitamin D than it does on calcium. (More on this later.) In fact, consumption of too much calcium is just plain damaging to your bones and your health in general. And with that in mind, let’s take a look at the calcium study that has everyone up in arms.
The study
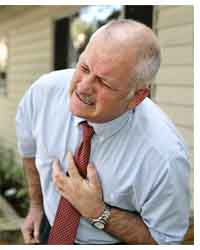 A little over two years ago, Dr. Ian Reid conducted research that unexpectedly showed a slight increase in heart attacks among healthy, older women who took calcium supplements to prevent fractures. This was surprising since, as Dr. Reid said, “Our hypothesis when we started the study was that calcium would protect the heart.”
A little over two years ago, Dr. Ian Reid conducted research that unexpectedly showed a slight increase in heart attacks among healthy, older women who took calcium supplements to prevent fractures. This was surprising since, as Dr. Reid said, “Our hypothesis when we started the study was that calcium would protect the heart.”
Stirred by this quirk in the data, Dr. Reid and his colleagues performed a meta-analysis of the existing data by combining and analyzing the findings from 11 randomized trials in which some 12,000 participants took calcium supplements (500 milligrams or more per day) without vitamin D. After adjusting for differences in study design, the researchers concluded that calcium supplementation was associated with a 20-30 percent increase in the risk for heart attacks.
If this data is correct (which it most likely is), millions of people who take calcium supplements in the hopes of lowering their risk for bone fractures may actually be increasing their risk of having a heart attack. As Dr. Reid says, “I think we need to seriously consider whether calcium supplementation is a good thing for most people, given that it is associated with a very small decrease in fracture risk.”
Incidentally, Dr. Reid thinks the problem is confined to the use of calcium supplements, which he believes contribute to artery disease by elevating blood levels of calcium too rapidly. If that’s the problem, then according to Dr. Reid’s hypothesis, calcium from food sources, which are absorbed more slowly, would not present the same problem. (That of course, as we’ve already discussed, would depend on what food sources we’re talking about.)
Not surprisingly, considering how much the food and dietary supplement industry has invested in the virtues of calcium, the study has drawn influential critics like substance-enhanced narcissists to a Burning Man event.
The study’s critics
The study has been quickly trashed by doctors in India, who argue that calcium supplementation might be a problem in the west where calcium intake has been optimized in the daily diet (I assume he’s referring to dairy intake), but that in India people require supplementation because they don’t get enough calcium in their diets. On the other hand, those same doctors acknowledge that the real problem is probably that Indians largely suffer from an acute deficiency of Vitamin D, which is required for the absorption of calcium.
 In an interview with WebMD, cardiologist John Cleland of the U.K.’s Hull York Medical School called the analysis “concerning but not convincing” in linking calcium supplementation to heart attacks. “Heart attacks are serious business, so you would expect to see an increase in mortality in supplement users along with heart attacks,” he says. “The fact that this wasn’t seen makes me wonder if this intervention is changing the perception rather than the reality of this outcome.”
In an interview with WebMD, cardiologist John Cleland of the U.K.’s Hull York Medical School called the analysis “concerning but not convincing” in linking calcium supplementation to heart attacks. “Heart attacks are serious business, so you would expect to see an increase in mortality in supplement users along with heart attacks,” he says. “The fact that this wasn’t seen makes me wonder if this intervention is changing the perception rather than the reality of this outcome.”
Cardiologist Nieca Goldberg, echoes Dr. Cleland when she says, “It is hard to understand how calcium could increase the risk for heart attack and not for stroke or death if this association is real,” she says. But then, the causes of heart attack and stroke are usually quite different so why should there be an automatic correlation?
Meanwhile, Dr. Kishore of the Isle of Man has jumped in with an audio blog telling people not to panic over the results of the calcium study.
But make no mistake; this is not just an issue for doctors. Remember, the entire alternative health industry is heavily invested in calcium — both as a nutritional supplement and as a functional food additive. So, not unexpectedly, spokespeople for the industry have jumped into the fray. Andrew Shao, PhD, Senior Vice President of Scientific & Regulatory Affairs for the Council for Responsible Nutrition, and Daniel Fabricant PhD, vice president of scientific regulatory affairs for the Natural Products Association, told NutraIngredients-USA.com that the results of the recent study go against years of research that show the benefits of calcium supplementation. Mr. Fabricant suggests that the authors of the research ‘cherry picked‘ the fifteen studies from hundreds of available research studies in the area. But do the results really go against years of research? As I’ve already pointed out, there is a plethora of research indicating that high calcium intake and that animal sources of calcium are both highly problematic — that is, unless you chose to “cherry pick” them out of the equation.
So what’s the real story on calcium supplementation?
My position on calcium
As I said before, I’m not a big fan of calcium supplementation for most people — either in pill form or as a component of high dairy intake. Although a necessary nutrient, it doesn’t perform as promised when taken in large amounts for bone health…and as we now know, heart health. In summary, there is an abundance of research that shows that a high consumption of calcium (supplement or diet) leads to heart disease, arthritis, disabling PMS (or PMDD as the TV ads have renamed it), and senility. So what’s going on?
As I mentioned earlier, it’s only since the 1950’s, and thanks to the dairy industry, that we consume high levels of calcium and that the Daily Value has been set so high (1000+ mg). In truth, until the 1950’s, mankind evolved and lived quite healthily on a low calcium diet (under 200 mg a day). And although they may have suffered from many diseases, one problem that most people, pre-calcium overload, did not have was weak bones. In fact, the bones of ancient people whose skeletons occasionally appear in peat bogs and frozen in glaciers tend to be highly dense and robust.
Osteoporosis
Research has shown that taking more calcium and drinking more milk actually contribute to osteoporosis and make it worse. Nevertheless, doctors don’t just tell people to continue doing these things — they tell us that it’s not working because we’re not doing enough. The simple truth is that the incidence of hip fractures (a good indicator of osteoporosis) in countries that have the highest dairy consumption in the world (like Norway, Sweden, and the United States) is 50 times greater than in countries like New Guinea and South Africa that have extremely low consumption of dairy products (and animal products in general). Bottom line: high calcium intake does not prevent osteoporosis. Therefore, we need to do even more???! To understand the actual causes of osteoporosis and why consuming high calcium foods and supplements actually make it worse, check out my natural health newsletter: Osteoporosis. And for more on the role calcium plays in bone building, check out The Calcium Question.
Okay, so maybe it doesn’t build bones as promised, but how could supplemental calcium be harmful?
The calcification of soft tissue
 The term calcification refers to the binding of calcium with phosphate to form hard bony structures. This is what builds strong bones and teeth. But when calcification occurs in soft tissue (anywhere other than the bones and teeth), it presents major health problems. It can lead to hardening of organs and tissue such as the heart and arteries, kidneys, brain, skin, joints, breast, pancreas, prostate, and ovaries, etc. This calcification occurs primarily as deposits that steadily grow bigger over time. Examples include plaque build-up in the arteries (calcium is a major component of arterial plaque), kidney stones, and hardening of the ovaries. As calcification builds up in any of these areas, it can trigger inflammation, autoimmune responses, infection, and the total shut down of the affected organ. In fact, 50% of all deaths in North America are caused by calcification and hardening of the arteries and by calcification of the heart valves.
The term calcification refers to the binding of calcium with phosphate to form hard bony structures. This is what builds strong bones and teeth. But when calcification occurs in soft tissue (anywhere other than the bones and teeth), it presents major health problems. It can lead to hardening of organs and tissue such as the heart and arteries, kidneys, brain, skin, joints, breast, pancreas, prostate, and ovaries, etc. This calcification occurs primarily as deposits that steadily grow bigger over time. Examples include plaque build-up in the arteries (calcium is a major component of arterial plaque), kidney stones, and hardening of the ovaries. As calcification builds up in any of these areas, it can trigger inflammation, autoimmune responses, infection, and the total shut down of the affected organ. In fact, 50% of all deaths in North America are caused by calcification and hardening of the arteries and by calcification of the heart valves.
Conclusion
If supplementing with calcium is detrimental to bone health — and health in general — then what should we take.
Magnesium, a better natural alternative
Without calcium, you cannot live, but without adequate amounts of magnesium to balance that calcium, you will find yourself falling victim to hardening of the arteries, arthritis, diabetes, and senility. Magnesium is the activating mineral for close to 400 different enzyme reactions in the body (that we know about) – more than any other mineral. Too little magnesium literally impacts your body negatively in hundreds of ways. And what makes the problem even worse is that magnesium is much harder for your body to absorb and utilize than calcium. This fact alone makes a joke of the standard 2:1 ratio of calcium to magnesium recommended by the medical establishment and found in most dietary supplements. But based on absorption, the ratio provided by most supplements is much closer to 6:1 or even 8:1 in favor of calcium — a very unhealthy ratio. And dairy at 10:1 calcium to magnesium is about the worst possible ratio imaginable.
In fact, the medical community has it bass akwards. Instead of consuming 2:1 calcium to magnesium, you should consume 2:1 magnesium to calcium…at the very least. That means that for most people no calcium supplementation is required at all. And because of the absorption issues associated with magnesium, minor supplementation of magnesium is advisable. However, the more dairy you consume, the more magnesium you must supplement with to balance it out.
The bottom line is that magnesium is the most important major mineral needed by your body, and unfortunately, the one that is most often depleted.
Vitamin D
The body needs vitamin D to absorb calcium. Without enough vitamin D, one can’t form enough of the hormone calcitriol (known as the “active vitamin D”). This in turn leads to insufficient calcium absorption from the diet. Unfortunately most people, including about forty percent of all children, are vitamin D deficient.
Vitamin K
Vitamin K regulates where calcium deposits in the body. It activates a group of amino acids called “Gla” (gamma-carboxyglutamic acid). The best known Gla protein is osteocalcin (Gla-OC). Vitamin K works by helping osteocalcin hold onto calcium, which is necessary for osteocalcin to be able to regulate where calcium goes in the body — into the bones and teeth and away from the arteries. The bottom line is that vitamin K keeps calcium in your bones and teeth instead of allowing it to deposit in your soft tissues, causing a hard calcium build-up.
Note: there are two forms of vitamin K, K1 and K2. You want K2. Human studies show that vitamin K2 is up to ten times more bioavailable than K1. In addition, vitamin K2 remains biologically active in the body far longer than K1.
Boron
Boron is involved in processes that build and repair joints, giving it an important role in the prevention of arthritis. Boron also helps to prevent tooth decay, again because of its involvement in the metabolism of other essential minerals. Its ability to regulate calcium, magnesium, and phosphorus not only protects bones but also helps to keep teeth strong and healthy. Its primary action on calcium is probably indirect…by activating vitamin D and estrogen. Studies have shown that postmenopausal women who took 3 mg of boron a day decreased the amount of calcium lost in their urine and increased their estrogen levels.
Essential fatty acids
Some studies suggest that EPA (Eicosapentaenoic acid, an omega-3 fatty acid) and GLA (gamma-linolenic acid, an omega-6 fatty acid) may help increase levels of calcium in the body and improve bone strength. In a study of women over 65 with osteoporosis, those who took EPA and GLA supplements had less bone loss over 3 years than those who took a placebo. Many of these women also experienced an increase in bone density.
In addition, several studies in the past decade have shown that EFAs (Essential Fatty Acids), when combined with calcium, can ensure that calcium deposition will take place in bone and not in the arteries, the kidneys, or other soft tissues. EFAs enhance the effects of vitamin D in the gut and improve calcium absorption from the small intestine, reduce the urinary excretion (loss) of calcium, increase calcium that is deposited in the bone, and improve the strength of bone.
The dosage required, for example, for evening primrose (GLA) to do this in both men and women is between 1500 — 6000 mg. daily. Of course, calcium uptake also depends to varying degrees on the frequency of weight bearing exercises (the more weight bearing exercise you do, the more calcium your body will deposit in the bone), as well as the presence of minerals such as magnesium, zinc, copper, strontium, silicon, manganese, and boron. If your calcium supplement does not contain evening primrose oil (and it probably does not), you might want to consider supplementing with an extra 1500 — 6000 mg. of this omega-6 source of essential fatty acids each day to help prevent or reverse bone loss.
pH
If you have not already done so, I suggest you read the chapter in Lessons from the Miracle Doctors that talks about “cleansing your blood” to get a better understanding of how a high acid diet (meat, fish, poultry, eggs, dairy, cooked grains, and refined sugars) leeches calcium from the body. But for now, the brief explanation is that when you consume a high acid diet, your body is forced to use calcium (from your bones or from your diet) to buffer the high acid content so that your blood pH remains constant and you don’t die. Incidentally, t
he problem with dairy, in addition to its 10:1 calcium to magnesium ratio, is that it actually takes more calcium to buffer its acid forming potential (from its high phosphorus content) then you actually receive from the dairy — thus the high incidence of osteoporosis in countries that consume a lot of dairy. Now, do not misunderstand. I am not saying that dairy is the biggest culprit in your diet. Actually, all of the other acid foods are worse — particularly high-sugar soda pop. I just single dairy out because it’s always identified as building strong bones, when the opposite is actually true.
So what is one to do? Well first, you might want to rethink your diet to minimize the intake of high acid forming animal foods (to less than 3 ounces a day) and the elimination of refined grains and sugars. At that point, the amount of highly absorbable calcium that you get in your diet from foods such as romaine lettuce, broccoli, sesame seeds, and bok choy, for example, will be more than adequate to build strong bones.
And for those who do not wish to modify their diet? Calcium supplementation is required so that the calcium used to buffer the acids produced in your body comes from outside sources rather than your bones. Coral calcium is not especially absorbable by the body (despite claims to the contrary). It’s pretty much just calcium carbonate, and there are better sources of calcium for building bones if you must supplement for that purpose. However, it is very effective at neutralizing excess acid and raising the pH of your soft tissue and fluids other than blood, so it is helpful at reducing the rate of bone loss. Just for fun, if you have some coral calcium in your house, pour a capsule into a can of sugared soda pop and watch what happens.
Of course, if you have the money, a water ionizer that splits water at your tap into acid water for washing and alkaline water for drinking is an even better choice as it allows you to precisely select the pH of the water you drink — giving you much better control of your body tissue pH levels. Another alternative is to expose water to a magnetic field, which also raises pH. The effect is nowhere near as strong as with a water ionizer, but it is much less expensive. And finally, you even have the option of adding alkalinizing drops to your water to raise pH.
Oral chelation
 Arterial calcification and the buildup of calcium in joints can be removed with oral chelation therapy. This treatment works by binding the calcium deposits in your joints and soft tissue so that they can be easily removed from your body.As more inappropriately placed calcium is removed from your body, joints feel looser and arterial plaque is dissolved and flushed from the body. The inflammation of tissues that attracts the buildup is also lessened by the body’s natural processes. Many people find that chelation helps a variety of conditions.Note: using a good proteolytic enzyme formula will significantly complement this process.
Arterial calcification and the buildup of calcium in joints can be removed with oral chelation therapy. This treatment works by binding the calcium deposits in your joints and soft tissue so that they can be easily removed from your body.As more inappropriately placed calcium is removed from your body, joints feel looser and arterial plaque is dissolved and flushed from the body. The inflammation of tissues that attracts the buildup is also lessened by the body’s natural processes. Many people find that chelation helps a variety of conditions.Note: using a good proteolytic enzyme formula will significantly complement this process.
For more on oral chelation to remove calcium build-up in soft tissue, check out Clinically Proven Oral Chelation. Note: don’t worry about chelation pulling calcium from your bones. You’re talking about removing a few grams of calcium from your body’s soft tissue. It does this by breaking the electrical bond that binds the calcium to that tissue. It has virtually no impact on the skeletal system, which is not held together by electrical bonding, but rather, is more like hardened cement.
Kidney formula
There are actually four types of kidney stones
- Calcium stones
- Uric acid stones
- Struvite or infection stones
- Cysteine stones
Calcium stones are the most common, and a good kidney formula will break them up and flush them from the body. But a well designed kidney formula doesn’t stop there. It will actually dissolve all four types of stones — not to mention gallstones and pancreatic sludge to boot.
Wrap up
The bottom line is that the latest study showing the potential dangers of calcium supplementation to the cardiovascular system should not have come as a major surprise. And if it weren’t for Henry C. Sherman, who got a huge grant from the dairy industry in the 1950’s and raised the dietary allowance for calcium from 500 mg to 800 mg for everyone, we wouldn’t be having this discussion today. But even worse, the RDA for adult women has continued to climb — from 800 mg to 1,000 mg, to 1,200 – 1,500 mg. And recently, some gynecologists have started recommending 2000 mg.
In any case, now you know the full story, including what to do about any excess calcium build-up you may have in your soft tissue, how to naturally build bone mass, what dietary supplements to use, and how to avoid osteoporosis.












Thank you so much Jon. When I
Thank you so much Jon. When I need anything clarified, I always turn to you for the answers. I trust your knowledge and really appreciate you sharing it.
I found you article to be
I found you article to be very informative. Thank you.
You know, it’s surprising how
You know, it’s surprising how few people comment on these articles, because you’re a very informative guy.
I am very interested in
I am very interested in knowing more about removing calcification in soft tissue as I am suffering with this issue in the form of calcific tendonitis. If there is a system that helps remove calcification, (Clinically Proven Oral Chelation), how do I get a hold of it. Many thanks.
Oral chelation will only pull
Oral chelation will only pull out trace amounts of minerals, which is enough when it comes to toxic elements that are only present in trace amounts, but not enough to make a difference in calcium levels which are present in massive amounts in the body. Instead, you might want to consider trying to change the way your body regulates where calcium is deposited by raising your body pH. If your body is too acid, it will pull calcium out of your bones and deposit that calcium throughout your body to buffer it.
I found this site after I
I found this site after I realized I had been getting too much Ca in diet and supplements. For the last year, I had begun to have pain in my bones, joints, and my hands hurt to both use them, and even as I slept, I had to keep turning them because of pain. Because of other health issues, I’ve spent many years researching nutrients when I couldn’t get help from doctors. I’m also a retired RN. I’ve reduced my Ca supplement, and increased my Mg intake to a 1:1 ratio, and already I feel so much better. A hip problem has gone away (I couldn’t climb stairs without a rail) and the hands no longer hurt. I’ll probably reduce the Ca further. I already take K2 and D. I’m in my 70″s and just want to verify that this article is right on point.
Thank you Virginia!
Thank you Virginia!
Calcium supplements taken
Calcium supplements taken with exercise, vitamin D, and magnesium are more dangerous than sixty years of sugar, opiates, and cigarettes? I’ll tell all the addicts right away.
High calcium should not cause
High calcium should not cause any problems when coming from the right natural sources. Dairy products are not among those and should be avoided as much as possible.
The last years I suffered from a bad tendinitis, elbow spurs and joint problems. According to the specialist only operation was left as an option for the tendinitis.
After reading “Dead doctors don’t lie” of Dr Joel Wallach, I added 8 grams of minerals from natural source (ocean algae) containing Mg, boron, and over 2 grams of calcium to my already healthy diet. All problems disappeared over a period of several months with a noticeable daily improvement. My very bad tendinitis is gone without any other treatment (and this time doing heavy work with my hand made no difference), and so are the elbow spurs and joint problems.
Thank you for the article!
Thank you for the article! What would you suggest for nephrocalcinosis?
I understand raising the ph for most calcium deposits is helpful, but have also read that an alkaline urine will make phosphorus deposits worse…. Since phosphorus is soluble in acidic urine and crystallizes in alkaline urine.
Please help me figure this out. Thank you!
For obvious legal reasons, we
For obvious legal reasons, we cannot diagnose or prescribe for specific medical conditions, merely provide information. With that said, Jon is adamant that you never want to make your body so alkaline that your urine goes alkaline. Your urine should be slightly acidic. http://www.jonbarron.org/article/physiology-urinary-system. Bottom line, you want to raise your pH to the point where you soft tissue is slightly alkaline, but not so far that your urine is too.